Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Although our recent research demonstrates that young adult Medicare beneficiaries (age 18-35) with lupus (SLE) have higher risk of 30-day rehospitalization, predictors specific to young SLE patients have not been evaluated. The objectives of this study are to assess the risk of and predictors for 30-day rehospitalization in young adults with SLE on Medicare compared to non-SLE and older SLE Medicare beneficiaries to inform targeted efforts for readmission reduction.
Methods: This retrospective cohort study utilized a 20% random sample of all adult hospitalizations in Medicare from 2013-2014. Inclusion required at least 1 year of continuous Medicare AB coverage before hospitalization; hospitalizations with a SLE diagnosis code were included in the SLE sub-cohort. Observations from HMO or Railroad beneficiaries or specialty care hospitals were excluded.
Thirty-day rehospitalization rates were calculated by age group among SLE and non-SLE patients. Initial generalized logistic regression clustered by individual estimated the odds of rehospitalization by age group, presence of SLE, and interactions between age group and SLE. Multivariable regressions were then performed within each SLE age group strata based on a priori and LASSO selected predictors of rehospitalization in young adults including socioeconomic, hospitalization, and comorbidity factors.
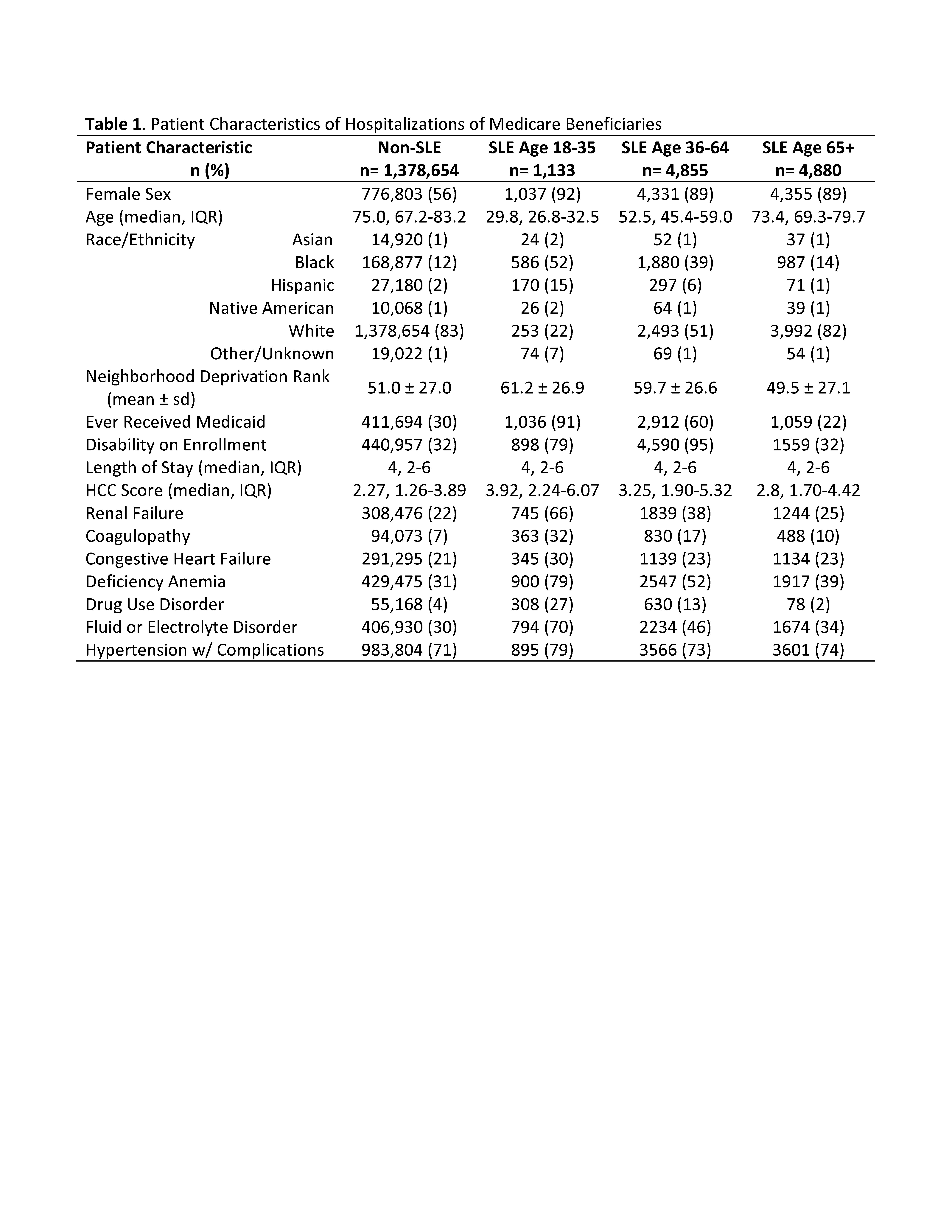
Results: Among 1,378,654 non-SLE and 10,868 SLE Medicare hospitalizations (Table 1), the observed 30-day rehospitalization rate in young adults without SLE was 26% (Figure 1). For young adults with SLE, the rehospitalization rate was 36%, decreasing to 20% in those over 65. Both young adult age (aOR 1.69, CI 1.60-1.78) and having SLE (aOR 1.18, CI 1.08-1.28) significantly increased odds of rehospitalization compared to patients of older age or without SLE; young adults with SLE had further increased odds (interaction term aOR 1.38, CI 1.11-1.71).
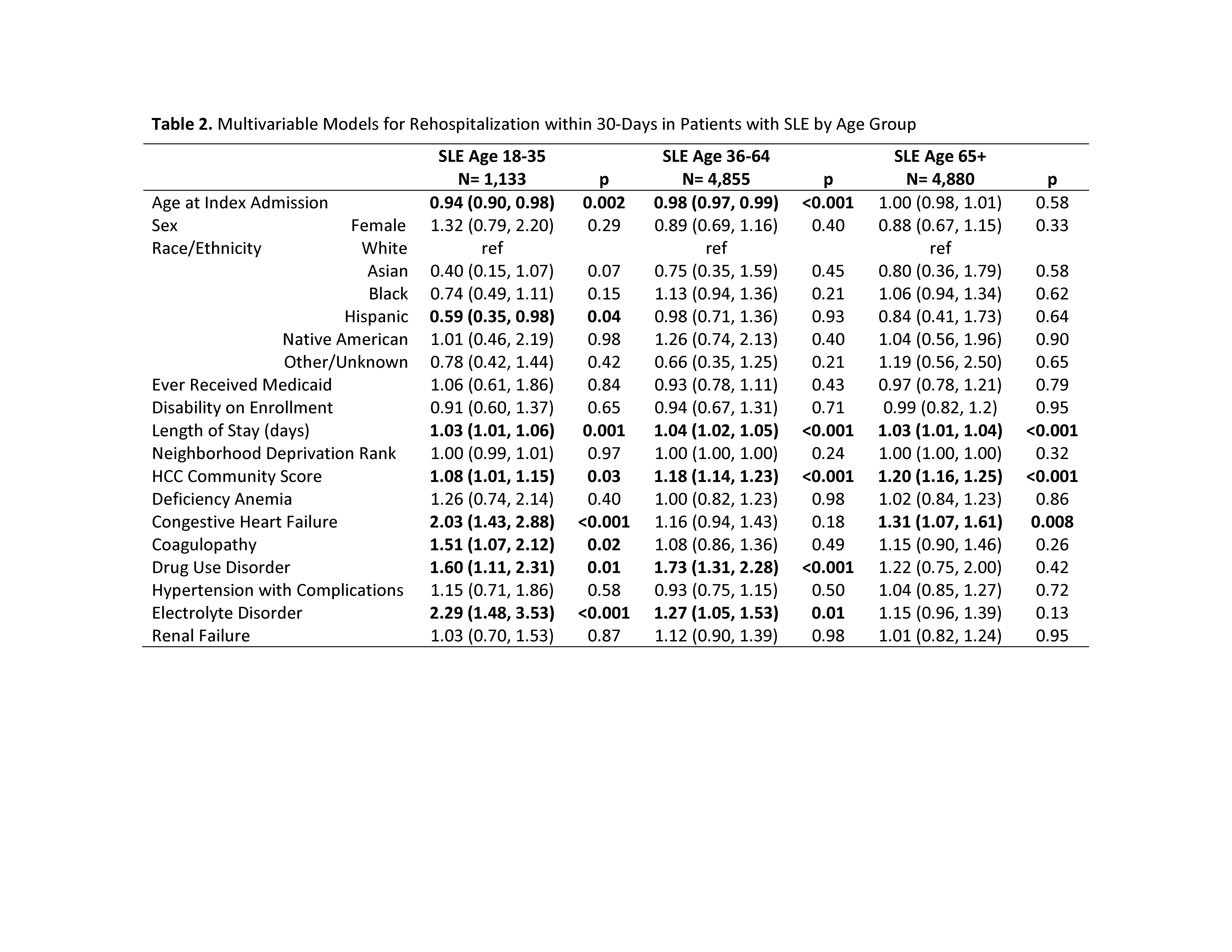
In multivariable models within age strata of SLE patients, each added day of index hospitalization length was associated with increased odds of rehospitalization in all age groups (Table 2). Among 18-64 year olds, increasing age was protective against rehospitalization. Medicare’s hierarchical condition category (HCC) score (designed to predict expenditures and mortality) was significantly associated with greater odds of rehospitalization in each age group, although the magnitude of effect was lower in young adults who had additional predictive factors such as heart failure, drug use, and coagulopathy.
Conclusion: Hospitalized young adults with SLE in the Medicare population are more racial diverse, from more disadvantaged areas, and have more comorbid conditions, and more than 1 in 3 are rehospitalized within 30 days of discharge. Comorbidities such as coagulopathy, drug use disorder, and heart failure conferred a greater increase in odds of 30-day rehospitalization in young adults with SLE than in older adults with SLE. Together these findings suggest a critical need to develop targeted interventions with young adults to support these high-risk patients and reduce rehospitalizations.
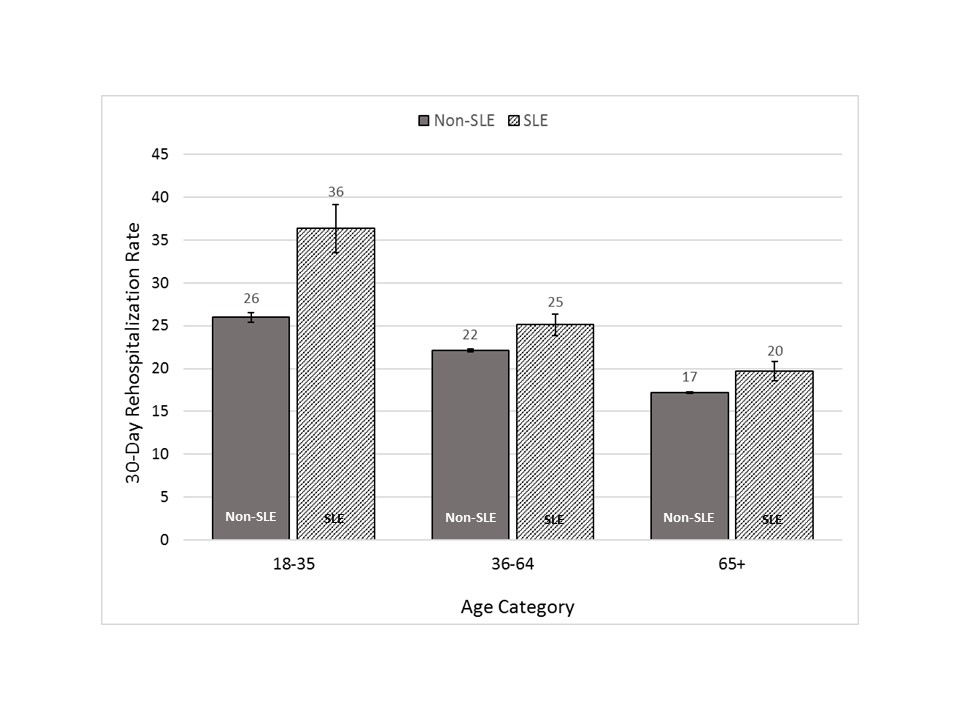 Figure 1. 30-Day Rehospitalization Rates by Age Group for Medicare Beneficiaries with and without SLE. Percentage of hospitalizations resulting in re-hospitalization within 30 days from discharge by age group among Medicare beneficiaries with (hatched bar) and without (solid bar) SLE. Error bars represent 95% confidence intervals.
Figure 1. 30-Day Rehospitalization Rates by Age Group for Medicare Beneficiaries with and without SLE. Percentage of hospitalizations resulting in re-hospitalization within 30 days from discharge by age group among Medicare beneficiaries with (hatched bar) and without (solid bar) SLE. Error bars represent 95% confidence intervals.
To cite this abstract in AMA style:
Schletzbaum M, Chen Y, Sheehy A, Kaiksow F, Powell R, Gilmore-Bykovskyi A, Kind A, Bartels C. Differences in 30-Day Rehospitalization Risk and Predictors by Age Group Among Patients with Lupus in Medicare [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/differences-in-30-day-rehospitalization-risk-and-predictors-by-age-group-among-patients-with-lupus-in-medicare/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-30-day-rehospitalization-risk-and-predictors-by-age-group-among-patients-with-lupus-in-medicare/