Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Ultrasound (US) of temporal (TA) and axillary arteries is recommended as the first imaging modality in patients with suspected predominantly cranial giant cell arteritis (GCA) and recently, two US scoring systems, the halo count and Halo Score, have been proposed to quantify the extent of vascular inflammation. We aim to assess the diagnostic value of both scoring systems and its association with systemic inflammation in patients with GCA seen in routine clinical practice.
Methods: This is a retrospective observational study including patients suspected of having GCA over a 9-month period. Baseline clinical and laboratory parameters were retrieved from the electronic health records. All patients underwent bilateral US examination of the three TA segments and extracranial (carotid, subclavian and axillary) arteries as part of a diagnostic fast track pathway (FTP). The FTP is offered to all patients with suspected GCA who will receive an appointment for the US examination within 24 hours. The extent of vascular inflammation was quantified according to the halo count (number of TA segments and axillary arteries with a halo) and the Halo Score (a composite index that incorporates the thickness of each halo). TA biopsy (TAB) was performed according to the treating clinician criteria. The gold standard for GCA was the clinical diagnosis after 6 months of follow-up by the treating clinician. Differences between groups were determined by Chi-squared and Student-t tests, validity was analyzed by receiver operating characteristic (ROC) curves and correlations were determined by Spearman’s rank correlation coefficient (rho).
Results: A total of 58 patients were evaluated in the FTP. Mean age was 74.7 years and 65.5% females. Clinical characteristics and US variables of patients with and without GCA are shown in Table 1. A clinical diagnosis of GCA was established in 15 (25.9%) patients. Only 4.7% patients without GCA versus 86.7% with GCA had positive US findings according to the ultrasonographer criteria (sensitivity (Sens) 86.7%, specificity (Spec) 95.3%, positive likelihood ratio (LR+) 18.4 and negative likelihood ratio (LR-) 0.14). Halo count and Halo Score showed similar diagnostic accuracy for a clinical diagnosis of GCA (area under the ROC curve of 0.892 and 0.921 respectively). The optimal cut-off point for halo count was ≥1 (Sens 80%, Spec 95.3, LR+ 17.02, LR- 0.21) and for Halo Score ≥2 (Sens 86.7%, Spec 95.3%, LR+ 18.4, LR- 0.14). Statistically moderate positive correlations were found between halo count and Halo Score and ESR (rho 0.385 and 0.325, p< 0.05) and CRP (rho 0.460 and 0.467, p< 0.01), but not with haemoglobin and platelet count (p >0.05) (Figure 1).
Conclusion: The extent of vascular inflammation by US halo count and Halo Score can help to support the diagnosis of GCA in routine care as they correlate with laboratory markers of systemic inflammation, mainly CRP. Although both scoring systems need further validation, they can be easily implemented in FTP of patients with GCA.
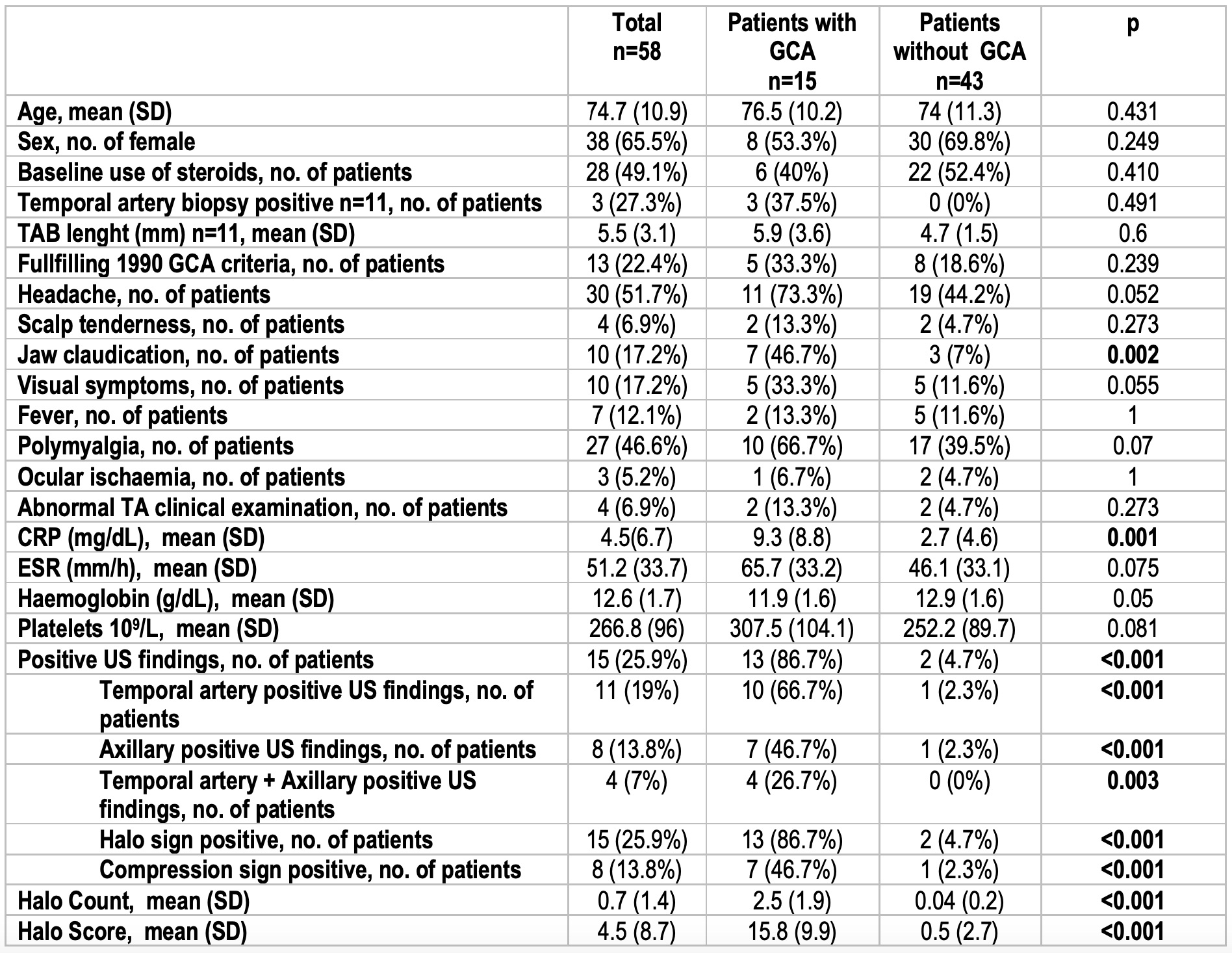 Table 1. Clinical, laboratory and ultrasound findings of patients included in the fast track pathway
Table 1. Clinical, laboratory and ultrasound findings of patients included in the fast track pathway
 Figure 1. Correlations between halo count and Halo Score with markers of systemic inflammation (ESR CRP, haemoglobin and platelets)
Figure 1. Correlations between halo count and Halo Score with markers of systemic inflammation (ESR CRP, haemoglobin and platelets)
To cite this abstract in AMA style:
Molina Collada J, Martínez-Barrio J, Serrano-Benavente B, Castrejon Fernandez I, Caballero Motta L, Trives Folguera L, Alvaro-Gracia J. Diagnostic Value of Ultrasound Halo Count and Halo Score in Giant Cell Arteritis: A Retrospective Study from Routine Care [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/diagnostic-value-of-ultrasound-halo-count-and-halo-score-in-giant-cell-arteritis-a-retrospective-study-from-routine-care/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-value-of-ultrasound-halo-count-and-halo-score-in-giant-cell-arteritis-a-retrospective-study-from-routine-care/
