Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) is a heterogeneous disease regarding its clinical expression, evolution and forms of presentation. In spite of the lack of a disease modifying therapy, there are effective treatment options to control complications such as pulmonary arterial hypertension (PAH), interstitial lung disease (ILD) or digital ulcers (DU). Early diagnosis is crucial and allows the physician to start these treatments as soon as possible. Our objetive is to study the main clinical manifestations that lead to diagnosis of SSc, the delay of the diagnosis after the beginning of the first symptom, and to analyze the role of the different clinical features in the diagnosis.
Methods: A retrospective and descriptive study was conducted, which included patients with SSc from our Rheumatology Department. Clinical data and specific autoantibodies profile (ACA, Scl-70, RNP) were recorded, paying special attention to the clinical manifestations that led to diagnosis. We classified them in eight categories: secondary Raynaud’s phenomenon (SRP), digital ischemia or DU, musculoskeletal symptoms, skin induration, ILD, PAH, specific autoantibodies detection, and others. The date of starting of Raynaud’s phenomenon (RP), of the first non-Raynaud symptom and the date when the diagnosis was established were registered. Analysis were conducted using STATA.
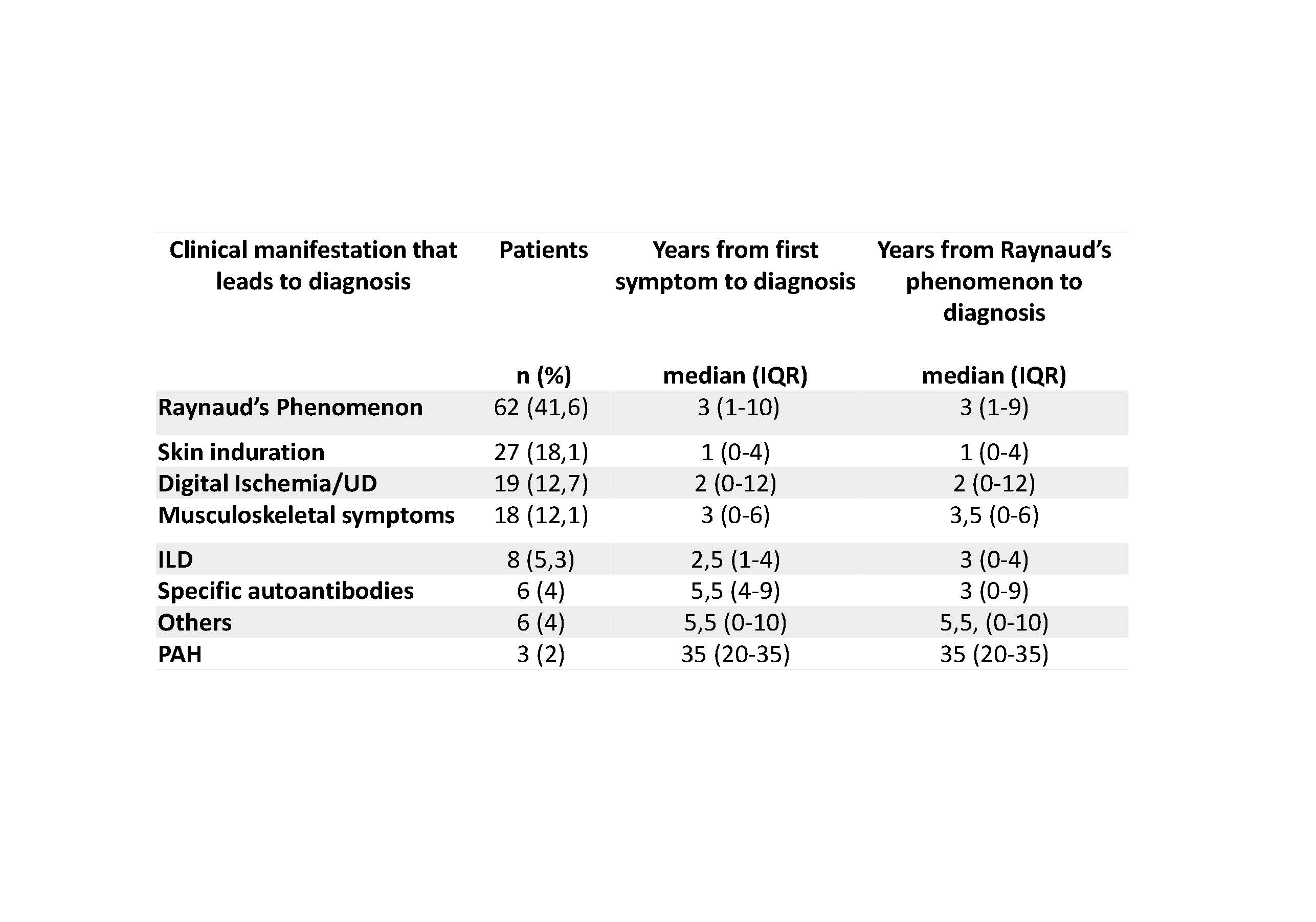
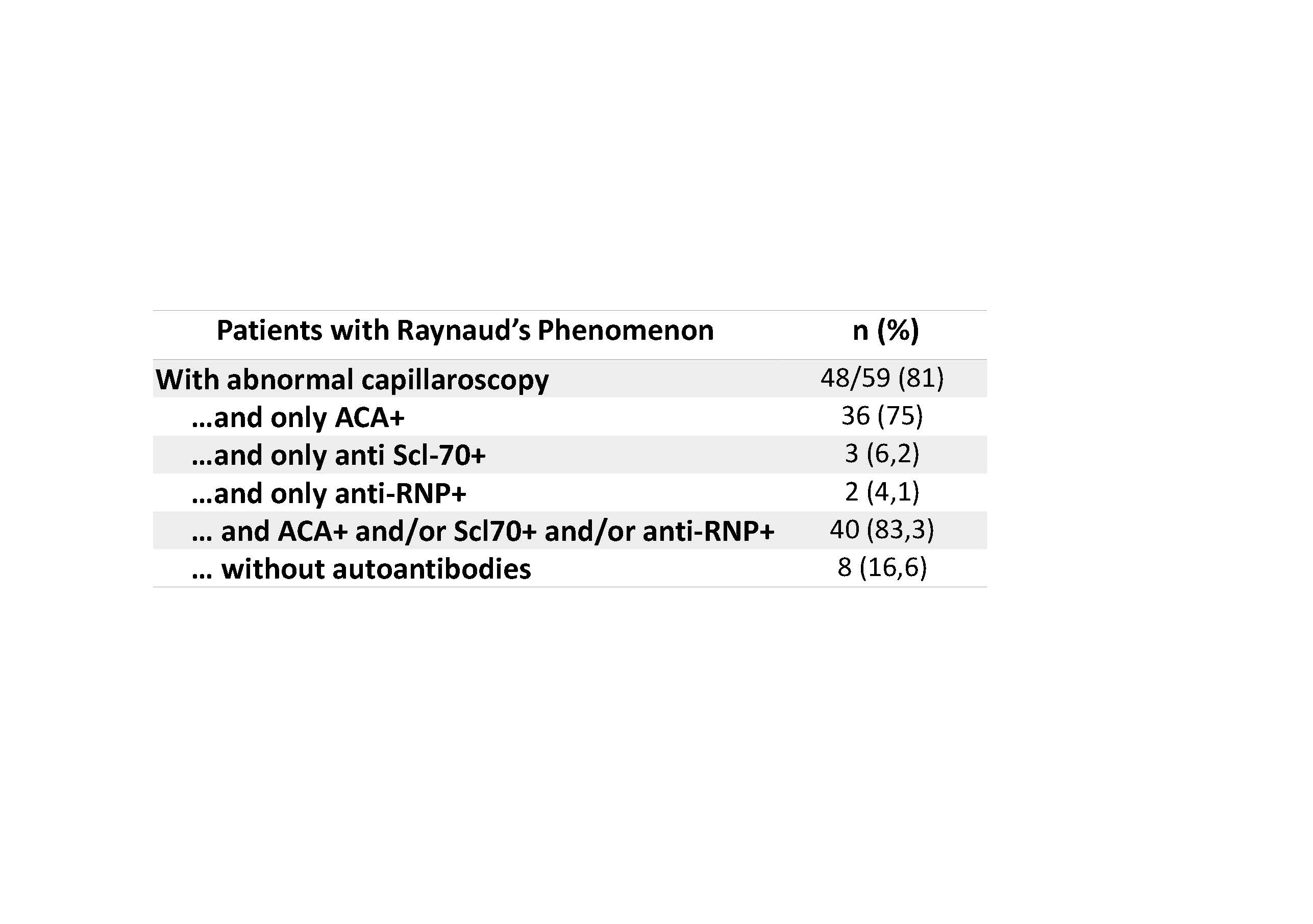
Results: The sample included 149 patients with SSc, meeting the 2013 ACR/EULAR criteria. RP appeared several years prior to the diagnosis (median of 3 years, IQR 0-8), and typically before the first non-Raynaud symptom. 141 out of 149 patients (94,6%) presented RP prior to the diagnosis. However, SRP was the manifestation that led to diagnosis in only 42/149 patients (41,6%), followed by skin induration (18,1%) and DU (12,7%). Surprisingly, 30/149 patients (20,1%) were diagnosed after the appearance of severe complications such as DU, ILD or PAH. Most patients started symptoms related to SSc several years before diagnosis (details in Table 1). 40/48 patients (83%) that were diagnosed due to SRP, presented abnormalities in nailfold capillaroscopy as well as specific autoantibodies (Table 2). Presenting telangiectasia, calcinosis, ILD or PAH was not associated with an early diagnosis, nor was ACA, Scl-70 or RNP positivity.
Conclusion: One out of five patients with SSc was diagnosed after the onset of complications. The study of RP by capillaroscopy and specific antibodies allows to reach the diagnosis of early SSc in up to 83% of patients. Early referral of patients with RP to the Rheumatologist and a multidisciplinary management of complications would improve the diagnosis of this potentially serious disease.
To cite this abstract in AMA style:
Sobrino C, De la Puente C. Diagnosis of Systemic Sclerosis: How and When [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/diagnosis-of-systemic-sclerosis-how-and-when/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnosis-of-systemic-sclerosis-how-and-when/