Session Information
Date: Monday, November 18, 2024
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders II
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: The aim of this study is to analyse the diagnostic value of the delay images at 180 minutes in positron emission tomography (PET) performed in patients with giant cell arteritis (GCA) despite glucocorticoid (GC) therapy before PET acquisition.
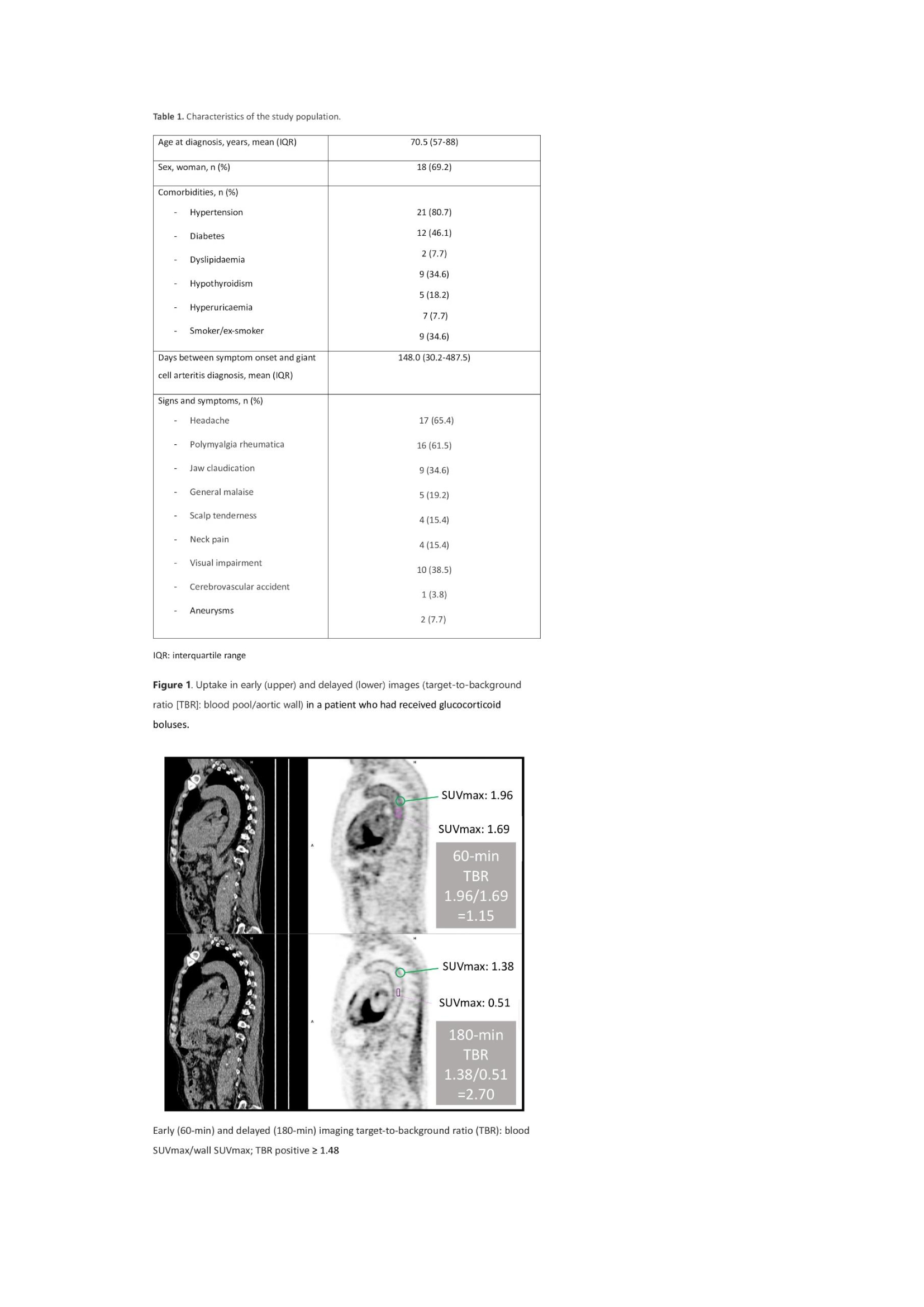
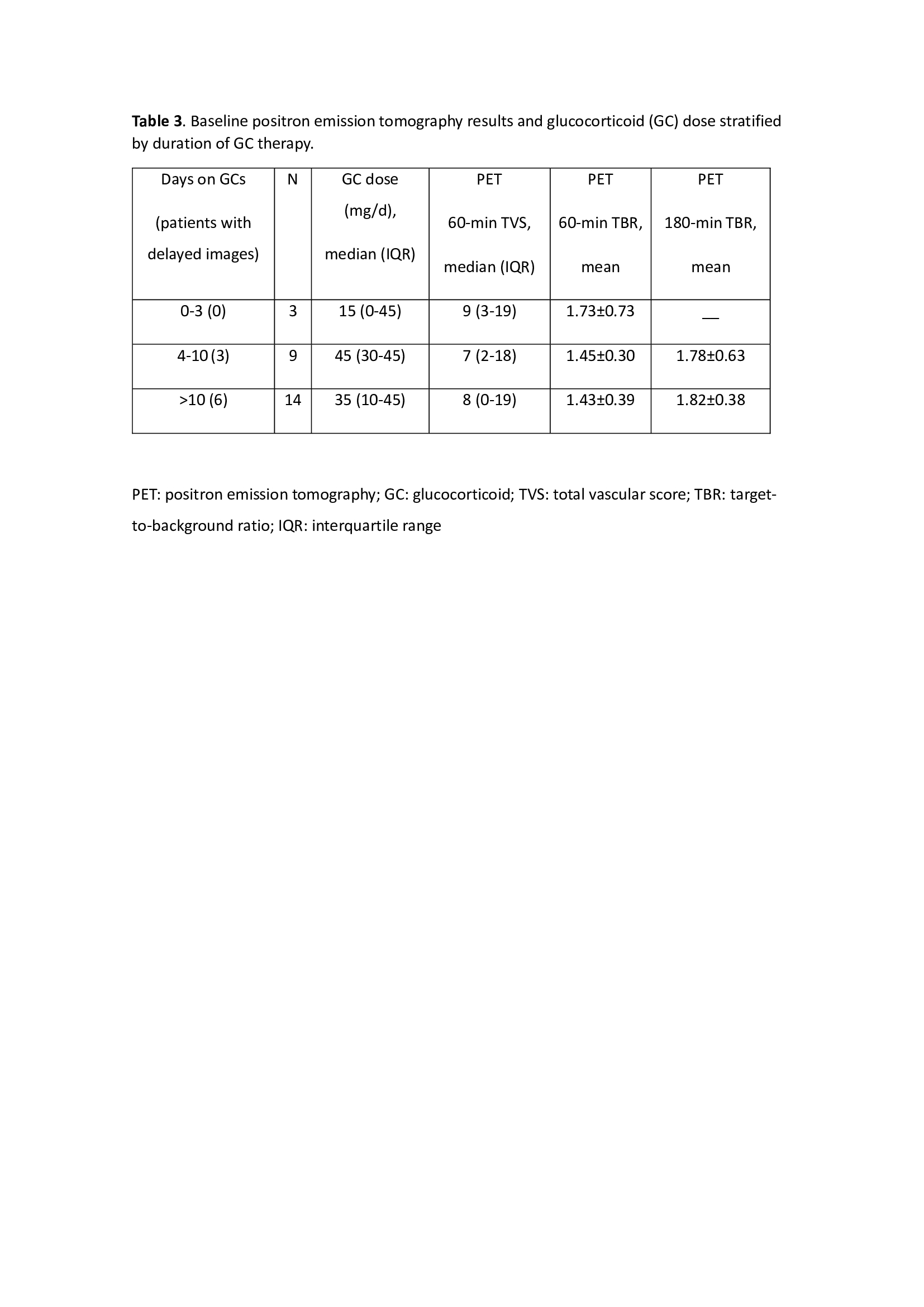
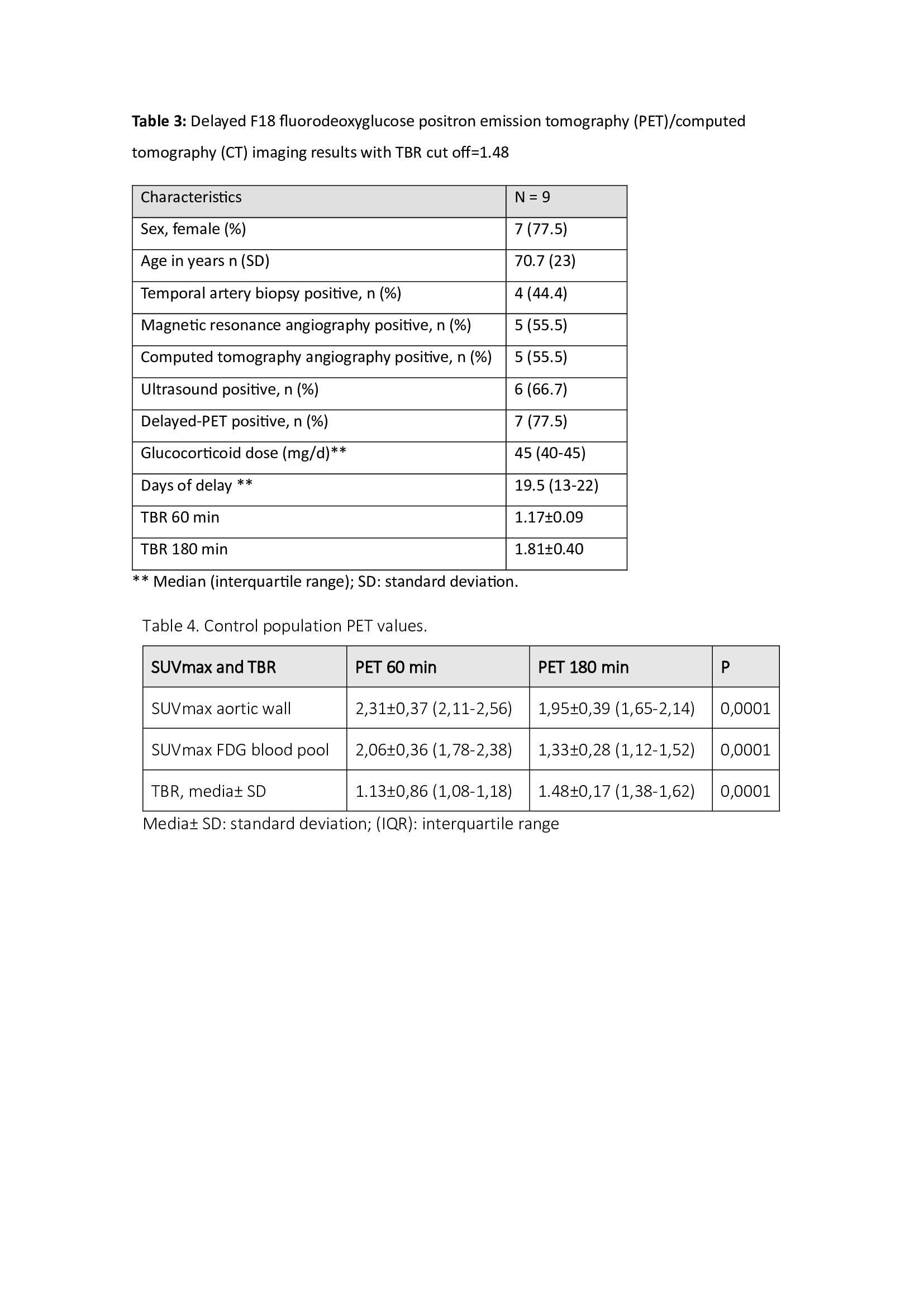
Methods: Consecutive diagnostic suspicious patients with GCA according to 2022 EULAR/ACR criteria as a reference standard were included. PET was performed at baseline and at 6 months. In patients with negative result at 60 minutes acquisition, delayed images were performed at 180 minutes. A total vascular score (TVS) was assessed at seven different vascular regions (thoracic aorta, abdominal aorta, subclavian arteries, axillary arteries, carotid arteries, iliac arteries, and femoral arteries). For semiquantitative analysis, volumes of interest (VOI) were drawn around the target arterial structures avoiding areas of atherosclerosis, and SUVmax at the liver and aortic wall to lumen ratio (corresponding to the TBR) were ascertained in both early and delayed acquisition, defining cut off for positivity of ≥ 1.48 according to our control population made with patients who underwent 18F-FDG PET/CT for suspected malignant lung nodules with a mean age of 71.6±8.9 (20 women and 5 men). Patients with a history of vasculitis and patients treated with chemotherapy or chemoradiotherapy in the previous 12 months were excluded.
Results: Twenty six patients were included with a median age of 70.5 (57-88) years. Baseline PET was positive in all but two: 17 patients at 60 min acquisition and 7 patients after delayed images at 180 min (table1 and figure1). The median dose of GCs at the time of the baseline PET was 45 mg/d (26.2-45) of prednisone-equivalent with a median exposure of 14 days (7-76.2) (table 3). Delayed images were perfomed in more patients with more time on GC treatment resulting in a sensitivity of 92,1% with a cutt off TBR ≥ 1.48 (table 4). At 6 months, the follow up PET was performed on 22 patients, with positive result in all but one, despite treatment with GCs and/or biological disease modifying antirheumatic drugs (bDMARD), although 18F-FDG uptake had decreased in all of them. Four patients died before the 6 month follow up PET: 2 due to pneumonia, 1 due to abdominal aortic aneurysm rupture and another for unknown reasons.
Conclusion: A PET scan beyond 3-10 days after treatment initiation may be useful, especially in patients with a strong suspicion of GCA. In this context, in patients under long term high dose GC treatment, delayed imaging applying procedural recommendations for vascular quantification could be of great interest in clinical practice. A TBR ≥ 1.48 could be a good cut off to diagnosed GCA by PET with a sensitivity of 92.1%. In line with this GC dose seems to be less relevant than the time on steroid treatment.
With this data we suggest to perform only one acquisition at 180 min in these kind of patients and in those with high suspicion of GCA and negative PET at 60 min.
1.- Martínez-Rodríguez I, et al. Aortic Nucl Med Commun. 2013 Sep;34(9):926-30.
2.- Martínez-Rodríguez I et al.. Eur J Nucl Med Mol Imaging. 2014 Dec;41(12):2319-24
To cite this abstract in AMA style:
Aldasoro V, Betech-Antar V, Castañeda S, De Miguel E, Rosales J, García Velloso M. Diagnosis of Giant Cell Arteritis by 18F-FDG PET/CT in Patients on Glucocorticoid Therapy: Importance of Delayed Imaging [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/diagnosis-of-giant-cell-arteritis-by-18f-fdg-pet-ct-in-patients-on-glucocorticoid-therapy-importance-of-delayed-imaging/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnosis-of-giant-cell-arteritis-by-18f-fdg-pet-ct-in-patients-on-glucocorticoid-therapy-importance-of-delayed-imaging/