Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Comorbidity risk is remarkably increased in patients with Systemic Lupus Erythematosus (SLE) compared with the general population. A better understanding of comorbidity development in SLE is needed to improve the prognosis in SLE patients. We assessed the accrual of comorbidity utilizing the Charlson Comorbidity Index (CCI) in a large nationwide cohort of patients with SLE compared with matched population controls.
Methods: We assembled a cohort of adult patients with incident SLE using ICD diagnosis codes registered in the Danish National Patient Register (DNPR) from January 1996 to July 2018 (n=3,178). The date of the first SLE registration in the DNPR was considered the baseline. SLE patients were age, – and sex-matched to 60,090 population controls randomly selected from the Danish Civil Registration System. Comorbidities (during outpatient and inpatient care) were identified using DNPR. We estimated the CCI score, number of CCI comorbidities and cumulative prevalence (%) of CCI comorbidities, stratified by sex, at baseline (SLE diagnosis) and at the end of follow-up (FU) (death, emigration or July 2018) in patients with SLE and controls.
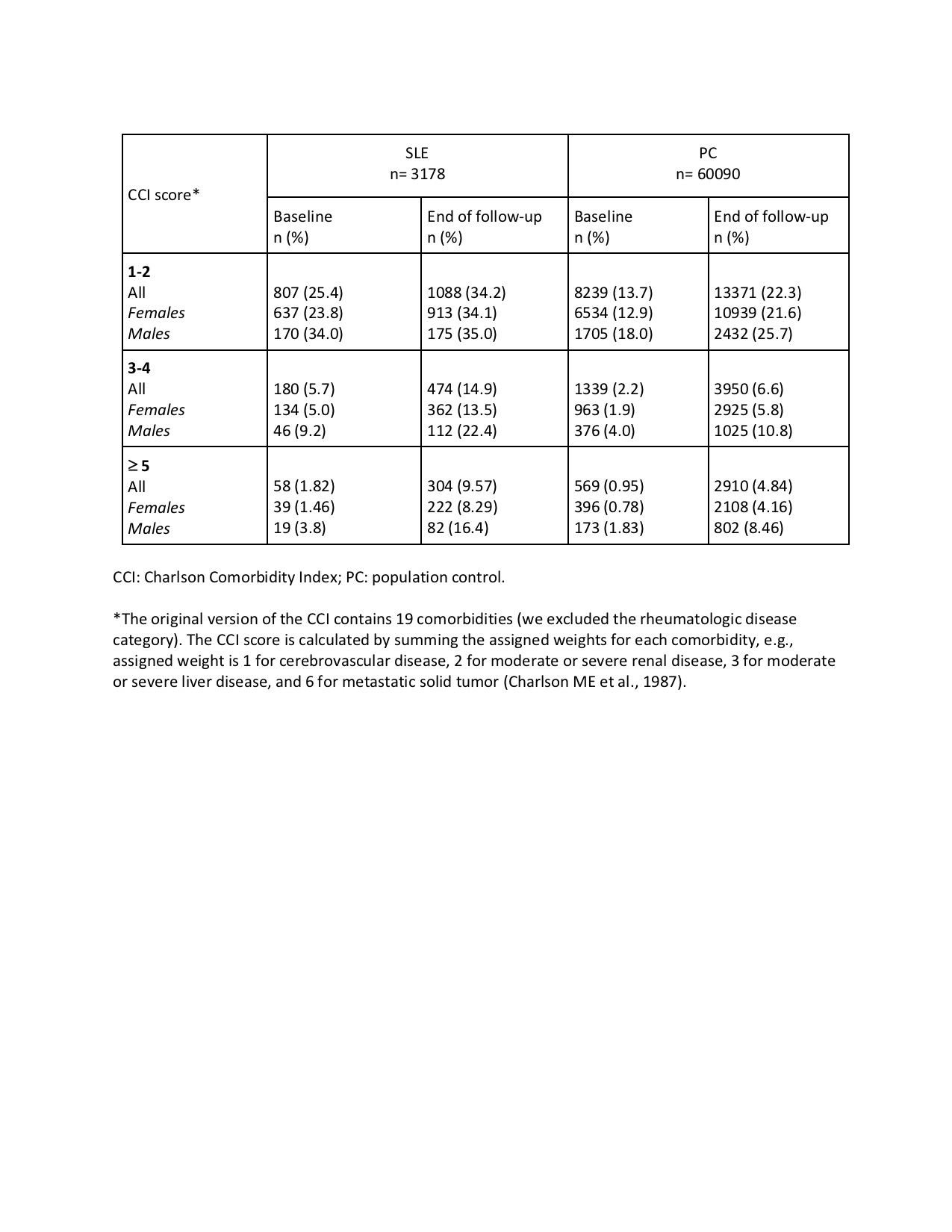
Results: 84% of SLE patients and non-SLE controls were female; mean age at baseline was 47 years. Mean CCI scores were 2.3 times higher in SLE patients vs controls at baseline (0.7 vs 0.3) and 1.9 times higher at the end of FU (1.7 vs 0.9). Similarly, the CCI scores were about 2-3 times higher in SLE patients than controls in the 1-2, 3-4 and ≥ 5 score categories, both at baseline and the end of FU (Table 1). Males had higher scores than females in all the above categories.
Number of CCI comorbidities
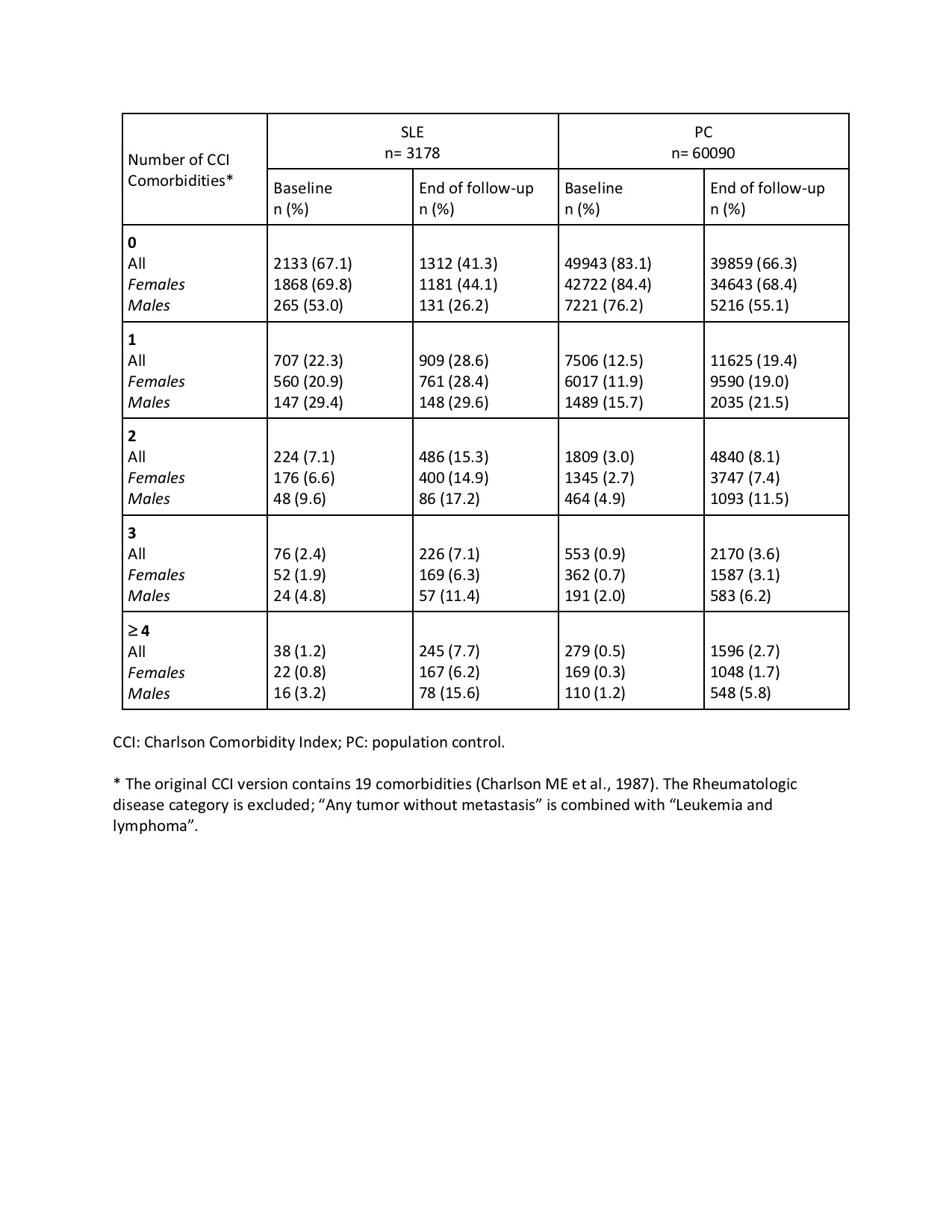
Fewer SLE patients than controls had no CCI comorbidities at baseline: 67% vs 83%, and at the end of FU: 41% vs 66% (Table 2). Two out of ten SLE patients had at least one CCI comorbidity at baseline vs one out of ten controls. Moreover, compared with controls, patients with SLE were 2-3 times more likely to have 2, 3 and 4 CCI comorbidities, at baseline and the end of FU.
Cumulative prevalence of CCI comorbidities
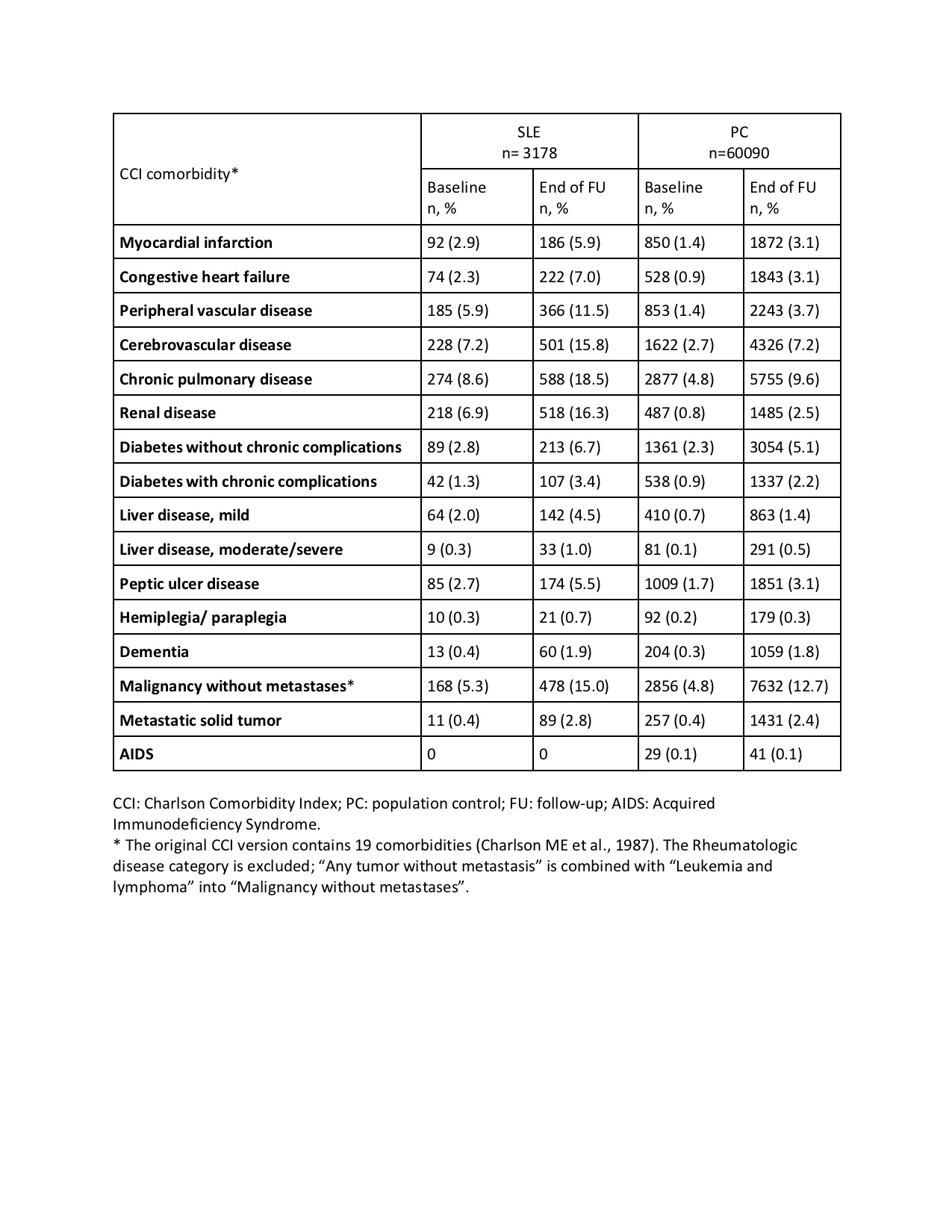
The cumulative prevalence of myocardial infarction, congestive heart failure, and peripheral vascular, cerebrovascular, chronic pulmonary and liver diseases was 2-4 times higher in patients with SLE than controls, at baseline and the end of FU (Table 3). Of note, in SLE patients, the cumulative prevalence of all the above comorbidities, as well as diabetes and peptic ulcer, doubled by the end of FU compared with baseline. Relative to controls, renal disease was the most prevalent comorbidity in SLE, with baseline and end-of-FU prevalence 8.6 and 6.5 times higher in SLE patients vs controls. Baseline and end-of-FU prevalence of malignancy was similar in SLE and controls. Most CCI comorbidities were more prevalent in males than females.
Conclusion: The baseline and end-of-follow-up cumulative prevalence of myocardial infarction, congestive heart failure, and renal, peripheral vascular, cerebrovascular, chronic pulmonary and liver diseases was substantially increased in patients with SLE compared with matched general population controls. The CCI scores and the number of CCI comorbidities were about 2-3 times higher in SLE patients than controls, at baseline and at the end of follow-up.
To cite this abstract in AMA style:
Baronaite Hansen R. Development of Charlson Comorbidity Index (CCI) Comorbidities and CCI Score in Danish Nationwide Cohort of 3,178 Patients with Newly Diagnosed Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/development-of-charlson-comorbidity-index-cci-comorbidities-and-cci-score-in-danish-nationwide-cohort-of-3178-patients-with-newly-diagnosed-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-charlson-comorbidity-index-cci-comorbidities-and-cci-score-in-danish-nationwide-cohort-of-3178-patients-with-newly-diagnosed-systemic-lupus-erythematosus/