Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: Alterations in nociceptive signaling, such as pain sensitization, which is an abnormal ascending pain facilitation, and/or inadequate descending pain modulation, are thought to be underlying mechanisms contributing to the transition from intermittent to constant pain in knee osteoarthritis (OA). Studies to date have primarily focused on individual measures of pain sensitivity, which can be assessed by quantitative sensory testing (QST). Whether combining pain sensitivity measures may provide better insights into the transition from intermittent to persistent pain than individual QST measures is not known. We therefore sought to develop a composite pain sensitivity index (PSI) based on QST measures that incorporates multiple aspects of nociceptive alterations and evaluated its relation to development of constant pain in knee OA.
Methods: We included subjects from the Multicenter Osteoarthritis (MOST) Study, a NIH-funded longitudinal cohort study of persons with or at risk of knee OA. We assessed Intermittent and Constant Osteoarthritis Pain (ICOAP) at baseline and two years later, and the following QST measures at baseline: i) pressure pain thresholds (PPT) at the wrist and patellae assessed with an algometer as the point at which pressure changed to slight pain; ii) temporal summation (TS) at the wrist using weighted probes; and iii) conditioned pain modulation (CPM) using PPT at the wrist as the test stimulus pre- and post-conditioning stimulus (forearm ischemia); CPM was computed as the post-PPT: pre-PPT ratio. Each QST measure was standardized and rescaled to 0-100 score, and then the PSI was created by taking the average of the summed scores of the four measures with equal weights, leading to PSI on a 0-100 scale. A lower PSI score represents greater pain sensitivity. Among participants at baseline who had intermittent pain of at least ‘mild’ severity occurring ‘sometimes’, we examined the relation of the PSI to the development of knee-specific constant pain by ICOAP two years later using logistic regression with GEE, adjusting for potential confounders. We repeated analyses for individual QST measures that were also standardized and rescaled to 0-100.
Results: 2737 participants (3031 knees) were included (mean age 64 ± 10, 58% female, mean BMI 29.4 ± 5.7). Over a two-year period, 6.7% developed constant pain. Each 10-unit increase in PSI score (signifying less pain sensitivity) was significantly associated with 33% lower odds of developing constant pain over 2 years (Table). In contrast, the magnitude of association for each individual QST measures was either smaller than that of the PSI score, or not associated with developing constant pain (Table).
Conclusion: The PSI score was associated with developing constant pain, whereas the individual QST measures had either smaller or null associations. This PSI score highlights the potential clinical relevance of multiple coexisting nociceptive signaling alterations to the pain experience in knee OA, and supports the importance of performing a global assessment of pain sensitization to capture the overall status of the nociceptive system.
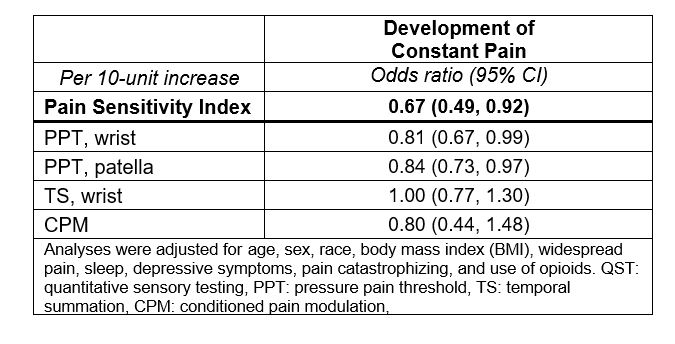 Table: Relation of PSI Score vs. Individual QST to Developing of Constant Pain Over Two-year Period
Table: Relation of PSI Score vs. Individual QST to Developing of Constant Pain Over Two-year Period
To cite this abstract in AMA style:
Aoyagi K, Carlesso L, Jafarzadeh S, LaValley M, Wang N, Frey Law L, Lewis B, Nevitt M, Neogi T. Development of a Pain Sensitivity Index to Examine the Transition from Intermittent to Constant Pain in Knee Osteoarthritis: The Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/development-of-a-pain-sensitivity-index-to-examine-the-transition-from-intermittent-to-constant-pain-in-knee-osteoarthritis-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-a-pain-sensitivity-index-to-examine-the-transition-from-intermittent-to-constant-pain-in-knee-osteoarthritis-the-multicenter-osteoarthritis-study/
