Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: To evaluate the patterns, severity and, prognostic parameters of interstitial lung disease (ILD) in Anti Jo1 Syndrome (AJS).
Methods: We identified 51 anti-Jo-1 patients with ILD between 2003 and 2012. Clinical and laboratory data were obtained along with PFTs and pattern/scoring of thoracic HRCT scans based on Ooi scoring system (inflammation and fibrosis indices) [1]. Progression of ILD was defined as follows: a decrease in DLCO and/or FVC (first to last reported) by >15%, an increase in fibrosis index or total HRCT score of ≥2, and death from respiratory failure.
Results: Of 51 patients; 20 were male and 15 had a diagnosis of dermatomyositis (DM). The median age at onset was 47 years, mean follow-up duration was 6.6 years; 3/15 (20%) presented with ILD prior to AJS diagnosis. Arthritis, mechanic’s hands, Raynaud phenomenon and fever were reported in 88%, 37%, 31%, and 23% of DM patients, respectively. Four patients had cancer: lung (1), prostate and gallbladder (1) and lymphoma (2). At diagnosis 3 patients had upper respiratory pneumonia, 13 (25%) had organizing pneumonia (3 with non-specific interstitial pneumonia (NSIP), with 5 developing NSIP later); 36 (70%) had NSIP: 22 fibrotic, 2 mixed and 12 cellular; 75% of cellular NSIP became fibrotic on subsequent imaging. Mean DLCO and FVC at diagnosis were 58.9% and 67%, respectively. The median initial inflammation and fibrosis indices at diagnosis were 5.6, 1.16 and at last follow-up 4.8, 2.1, respectively. Among 45 patients with available follow-up data; 17 had worsening ILD (39%) and 5 (11%) died of respiratory failure. A lower DLCO at diagnosis of DM was a predictor of disease progression [50 vs. 65% (p=0.0290)]. All upper respiratory pneumonia patients progressed during follow-up. Only 7 patients had a late diagnosis of ILD (≥3 years after onset of AJS). Of those, 5 (70%) had a DLCO ≤50% compared to a DLCO of 25% in those with early diagnosis. Sjögren’s syndrome antibody (SSA) positivity was detected in 53% of patients; lower initial (53% vs. 62%) and last (56% vs. 67%) DLCO as well as higher fibrosis score at last follow-up [3.5 vs. 0.9 (p=0.089)] were observed in SSA negative group. These differences did not reach statistical significance. Interestingly; 6/7 patients who died were SSA negative. Nine patients who developed pulmonary hypertension had higher median disease duration (10 years) and CT score (12.5) and all of them had DLCO ≤50%. Esophageal disease other than dysphagia was detected in 43% [GERD (33%), abnormal manometry or gastric emptying (15%) and dilatation on chest CT (10%)]. Esophageal disease trended towards lower DLCO at diagnosis [53 vs. 62% (p=0.084)], higher fibrosis score [2.7 vs. 1.6 (p=0.089)] and higher %change of total CT score [1.1 vs. -0.7 (p=0.007)].
Conclusion: Lower DLCO at diagnosis was associated with progression of ILD. The lower DLCO observed in late onset ILD may suggest a silent disease and reemphasizes the role of screening for ILD in AJS. In contrast to previous studies; SSA co-positivity was not associated with an adverse outcome. Esophageal disease seemed to be prevalent in anti-Jo-1 patients with ILD and may predict worsening fibrosis. However, the association of malignancy with anti-Jo1 syndrome (AJS) was not significant.
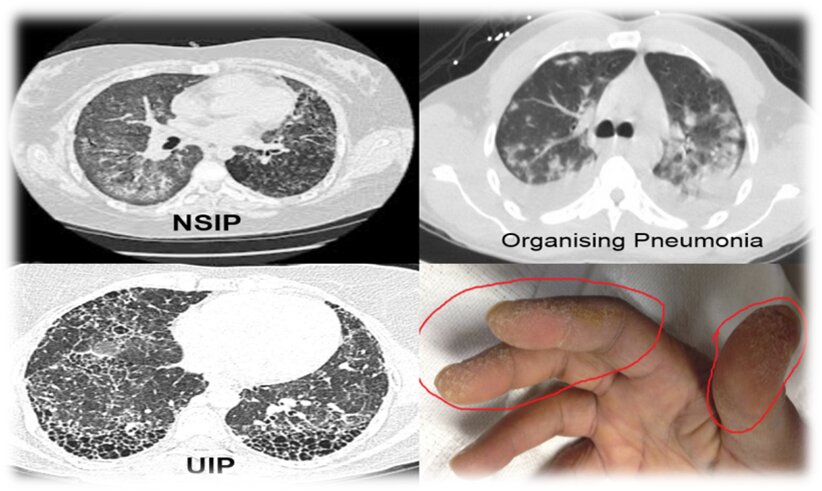 ILD patterns and Mechanic’s hands in AJS
ILD patterns and Mechanic’s hands in AJS
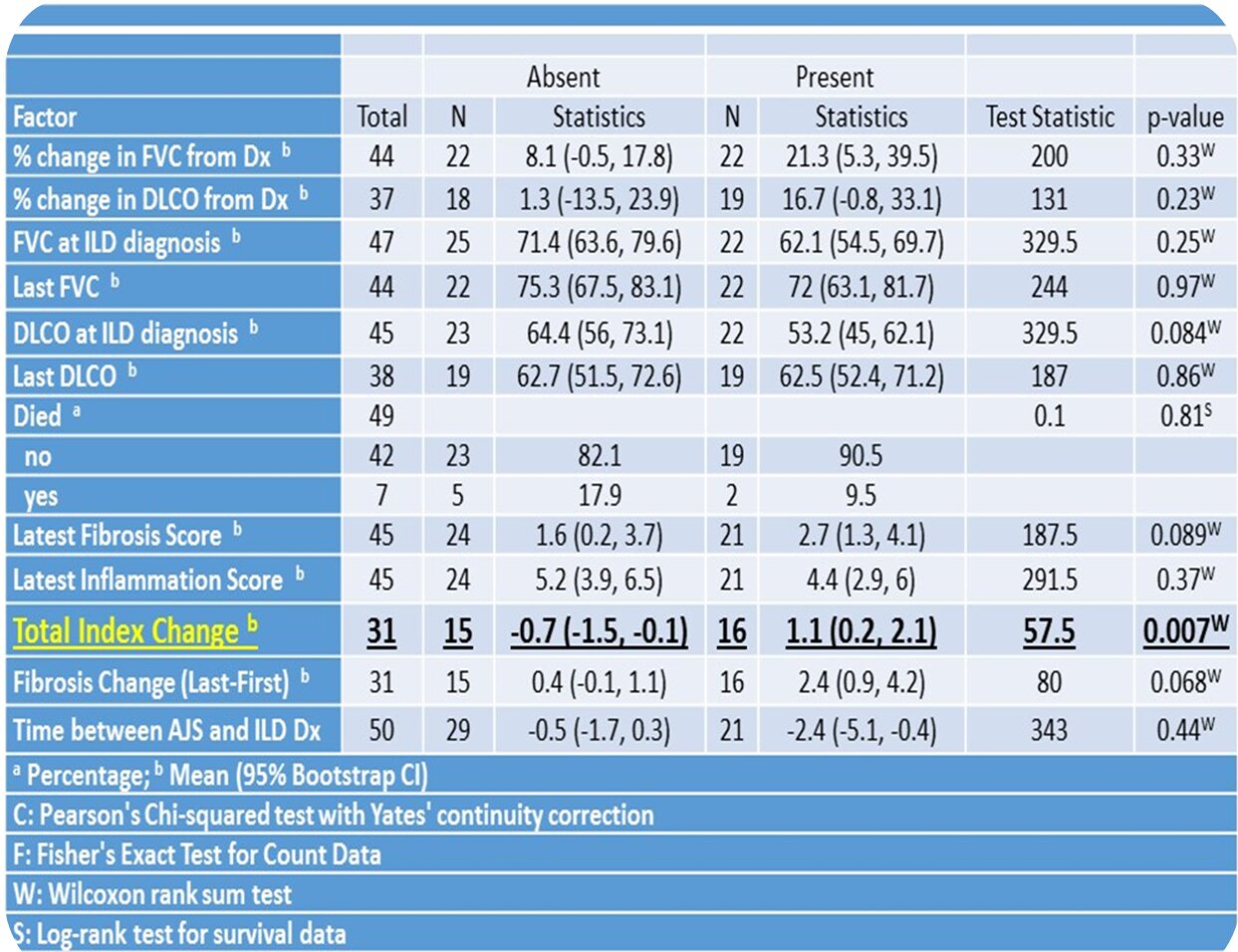 Table: Comparisons by Esophageal Disorder
Table: Comparisons by Esophageal Disorder
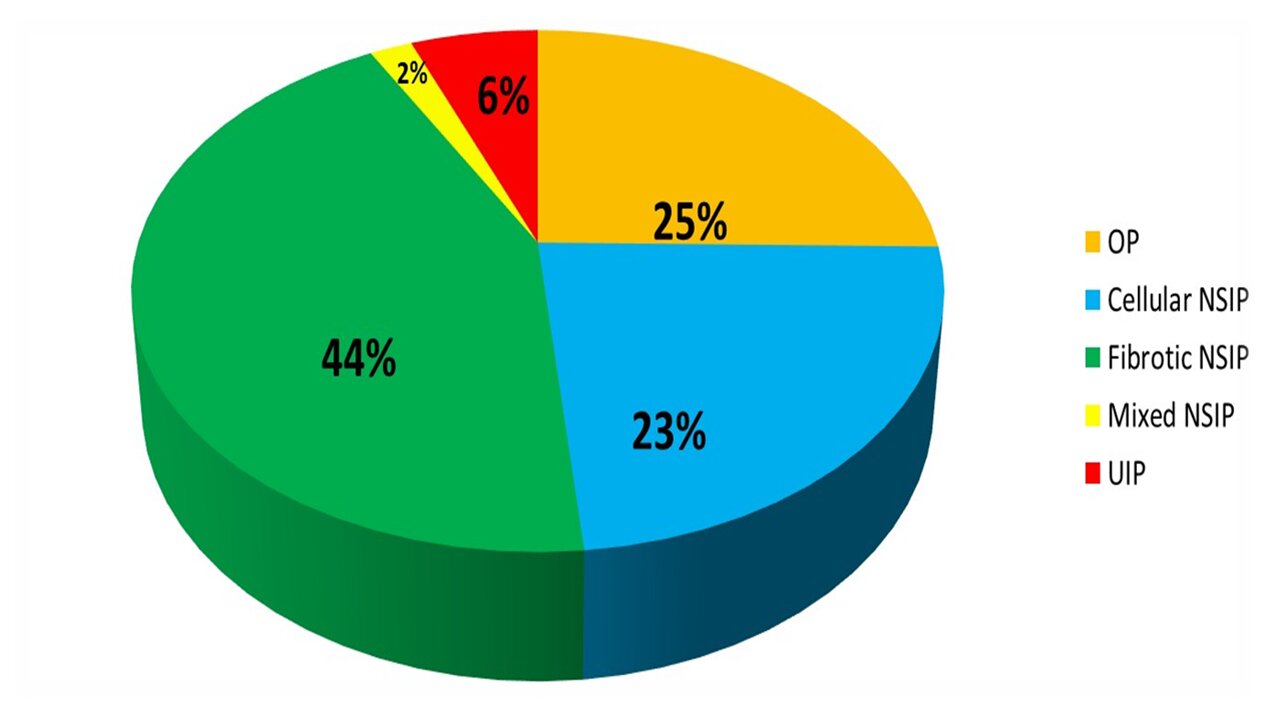 Patterns of ILD in AJS at diagnosis
Patterns of ILD in AJS at diagnosis
To cite this abstract in AMA style:
Alalwani M, Alhaddad B, Zraik B, O'Rourke C, Yadav R, Askari A, Malemud C, Chatterjee S. Descriptive Data Analysis of Patients with Anti Jo1 Syndrome (AJS) and Lung Involvement [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/descriptive-data-analysis-of-patients-with-anti-jo1-syndrome-ajs-and-lung-involvement/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/descriptive-data-analysis-of-patients-with-anti-jo1-syndrome-ajs-and-lung-involvement/
