Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Autoimmune diseases are complex conditions that may predispose individuals to an increased mental health burden, including depression. The immune system leads to inflammation in affected organs and mediates behavioral abnormalities, including fatigue and depression-like symptoms. This study leverages data from the Behavioral Risk Factor Surveillance System (BRFSS) to evaluate the prevalence of depression and mental health service access among patients with autoimmune diseases compared to those without.
Methods: Using a simulated BRFSS dataset of 10,000 respondents, autoimmune status was defined as the presence of conditions such as rheumatoid arthritis, lupus, and psoriatic arthritis. Depression was measured using self-reported ever diagnosis (ADDEPEV2) and the number of days of poor mental health (MENTHLTH). Descriptive analyses quantified the prevalence of depression in autoimmune versus non-autoimmune groups. Bivariate analyses (chi-square tests and t-tests) were conducted to compare mental health indicators and access to services between groups. Multivariable logistic regression models, with depression as the outcome and predictors including autoimmune status, demographics (age, sex, race/ethnicity, education, income), and comorbidities, were implemented. Stratified analyses by income further evaluated disparities in mental health care.
Results: Preliminary analyses indicated that 36% of respondents with autoimmune diseases self-reported depression compared to 21% among non-autoimmune respondents (χ² p < 0.001). Additionally, individuals with autoimmune conditions reported an average of 11.2 poor mental health days, significantly greater than the 6.3 days reported by non-autoimmune individuals (t-test, p < 0.001). Logistic regression analyses revealed that, after adjusting for demographic and comorbidity factors, the odds of reporting depression were 1.85 times higher among autoimmune patients (OR = 1.85; 95% CI: 1.60–2.15). Stratified analyses further demonstrated that lower-income autoimmune patients experienced compounded disparities; those in the lower-income bracket had an OR of 2.05 (95% CI: 1.70–2.47) compared to an OR of 1.62 (95% CI: 1.35–1.95) for their higher-income counterparts.
Conclusion: These findings suggest that individuals with autoimmune diseases have a significantly higher burden of depression and poorer mental health outcomes than those without. Moreover, the observed disparities in mental health service access, particularly among lower-income groups, underscore the need for targeted interventions to address these inequities. Future research should continue to explore the socio-demographic determinants affecting mental health service access in this vulnerable population.
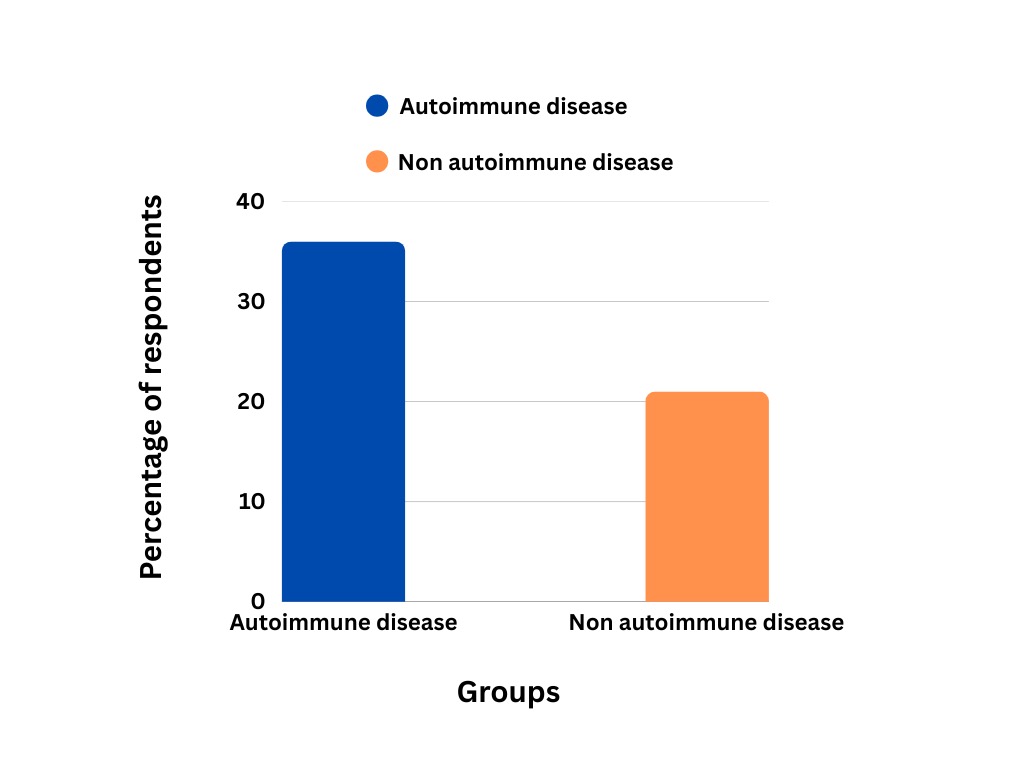 A graph comparing the percentage of respondents with depression in autoimmune disease group versus non-autoimmune disease group
A graph comparing the percentage of respondents with depression in autoimmune disease group versus non-autoimmune disease group
.jpg) A graph comparing the average poor mental health days in people with autoimmune disease versus non-autoimmune disease
A graph comparing the average poor mental health days in people with autoimmune disease versus non-autoimmune disease
To cite this abstract in AMA style:
Rathod M, Modi S, Kurra V, Yagnik K, Du D. Depression and Mental Health Service Gaps in Autoimmune Disease: Insights from a Simulated BRFSS Dataset [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/depression-and-mental-health-service-gaps-in-autoimmune-disease-insights-from-a-simulated-brfss-dataset/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/depression-and-mental-health-service-gaps-in-autoimmune-disease-insights-from-a-simulated-brfss-dataset/
