Session Information
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: Guidelines recommend osteoporosis screening using dual-energy X-ray absorptiometry (DXA) in men and women at risk for osteoporosis, but screening remains low, especially in men and in rural populations. System level approaches to aid in identification of at-risk populations have been suggested to close this clinical gap. An informatics-driven population health clinic, the “Bone Health Team” (BHT) was implemented to identify and treat rural Veterans lacking evidence of bone health care. We report the results of our process evaluation conducted to understand BHT feasibility.
Methods: The primary outcome of the process evaluation was the number of at-risk Veterans screened with DXA; a secondary outcome was the number of eligible Veterans who initiated prescription therapy to reduce fracture risk. Outcomes were measured between 5/1/2017-9/30/2018 and analyzed descriptively. Qualitative data to understand successful implementation were collected concurrently by conducting in-person interviews with clinical personnel interacting with BHT, interviews with BHT staff, and observations of BHT processes at three site visits. Data analyses followed the Promoting Action on Research Implementation in Health Services (PARIHS) Framework to characterize context, evidence, and facilitation.
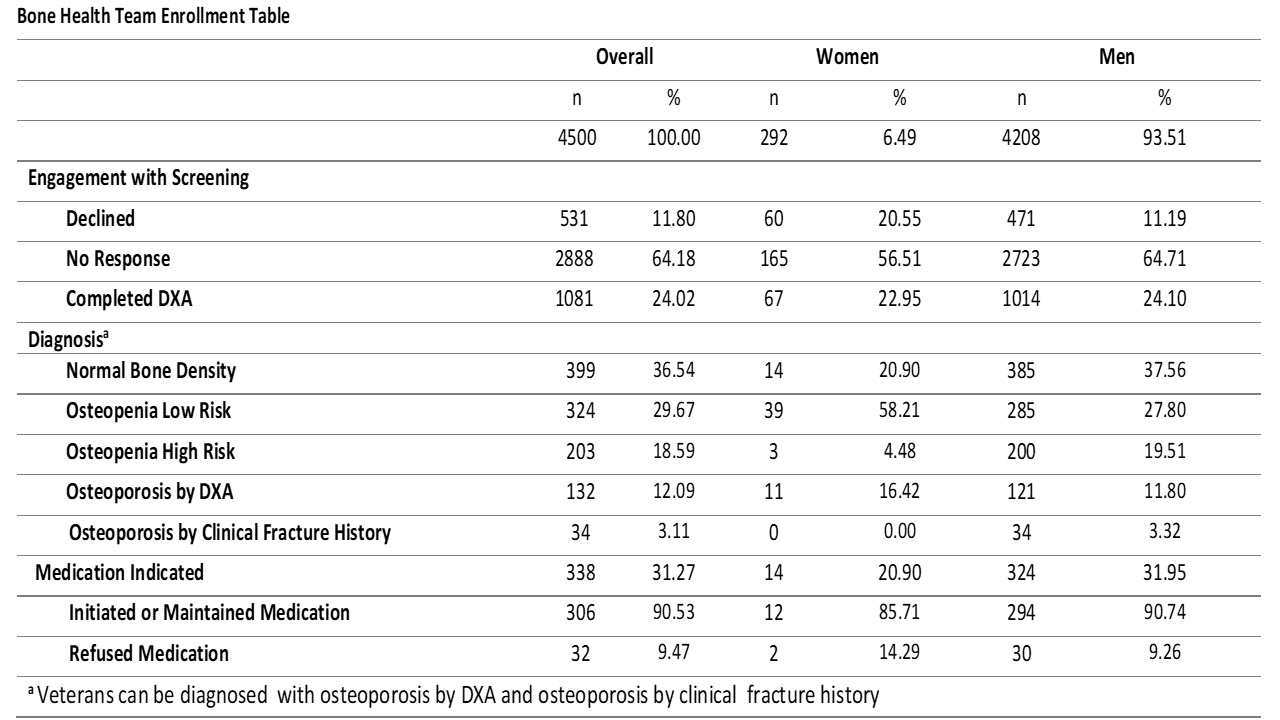
Results: Of the 4500 rural Veterans identified for osteoporosis screening, 292 (6%) were women, and 1081 (24%) completed screening (Table). Among these Veterans, 399 (37%) were found to have normal bone density, 527 (48%) osteopenia, and 156 (14%) osteoporosis with 338 (31%) eligible for prescription therapy to reduce fracture risk (Table). Of the Veterans eligible for prescription therapy, 306 (90%) initiated pharmacotherapy. Qualitative analysis identified contextual factors of rural geography and population characteristics including rugged terrain, harsh seasons, long distances between services, and limited access to cellular, internet, and mail services as barriers to the potential for travel, communication, and care delivery. The primary evidence factor acting as an implementation barrier was implementation complexity due to the requirement of significant infrastructural resources to sustain BHT processes. Factors of facilitation and evidence such as data infrastructure, evidence base for care delivery, stakeholder buy-in, formal and informal facilitator engagement, and focus on teamwork facilitated BHT implementation and expansion success.
Conclusion: The population telehealth model employed by the BHT is a feasible approach to delivering preventative osteoporosis care to rural Veterans and identified 31% of at-risk rural Veterans as eligible for prescription therapy to reduce fracture risk with 90% of those eligible choosing to initiate prescription therapy. The identified barriers and facilitators to implementing this model in the VHA will inform future model refinement and efforts to improve bone health care delivery systems for the Veteran population. Further evaluation to understand why more Veterans do not engage when offered osteoporosis screening, as well as the clinical and sociodemographic factors that predict Veteran acceptance of osteoporosis care, is ongoing.
To cite this abstract in AMA style:
Miller K, Steffen M, Seaman A, Anderson Z, Green J, Patel S, Wardyn S, Solimeo S. Delivering Fracture Prevention Through Telemedicine: A Process Evaluation [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/delivering-fracture-prevention-through-telemedicine-a-process-evaluation/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/delivering-fracture-prevention-through-telemedicine-a-process-evaluation/