Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Delays in access to specialized care and diagnosis of systemic lupus erythematosus (SLE) are associated with poor outcomes. Prior studies rely mostly on cross-sectional surveys and are probably subjected to recall bias. Moreover, Insufficient data from population-based SLE cohorts in the United States limits our understanding of delays to care. We aimed to (1) assess delays to access specialized care and diagnosis, (2) Identify characteristics associated with delays among patients with SLE.
Methods: We assembled a retrospective population-based cohort of adults with incident SLE from 1976 to 2018 in a 27-county region from the American Upper Midwest. All patients met the 2019 EULAR/ACR SLE criteria. Through medical records review, we identified the first medical contact where a manifestation attributed to SLE was noticed and mapped the patient’s trajectories and time to 1) first visit in specialized care (with rheumatology, dermatology, or nephrology) and 2) physician-diagnosed SLE. Disease activity (SLEDAI-2k) and SLICC/ACR damage indexes (SDI) were assessed at the classification date. Those patients who reached specialized care or were diagnosed ≥ 6 months after the first medical encounter were considered to have a delay. We compared demographics, first specialty seen and first clinical feature, SLEDAI, and SDI scores between groups with and without delays.
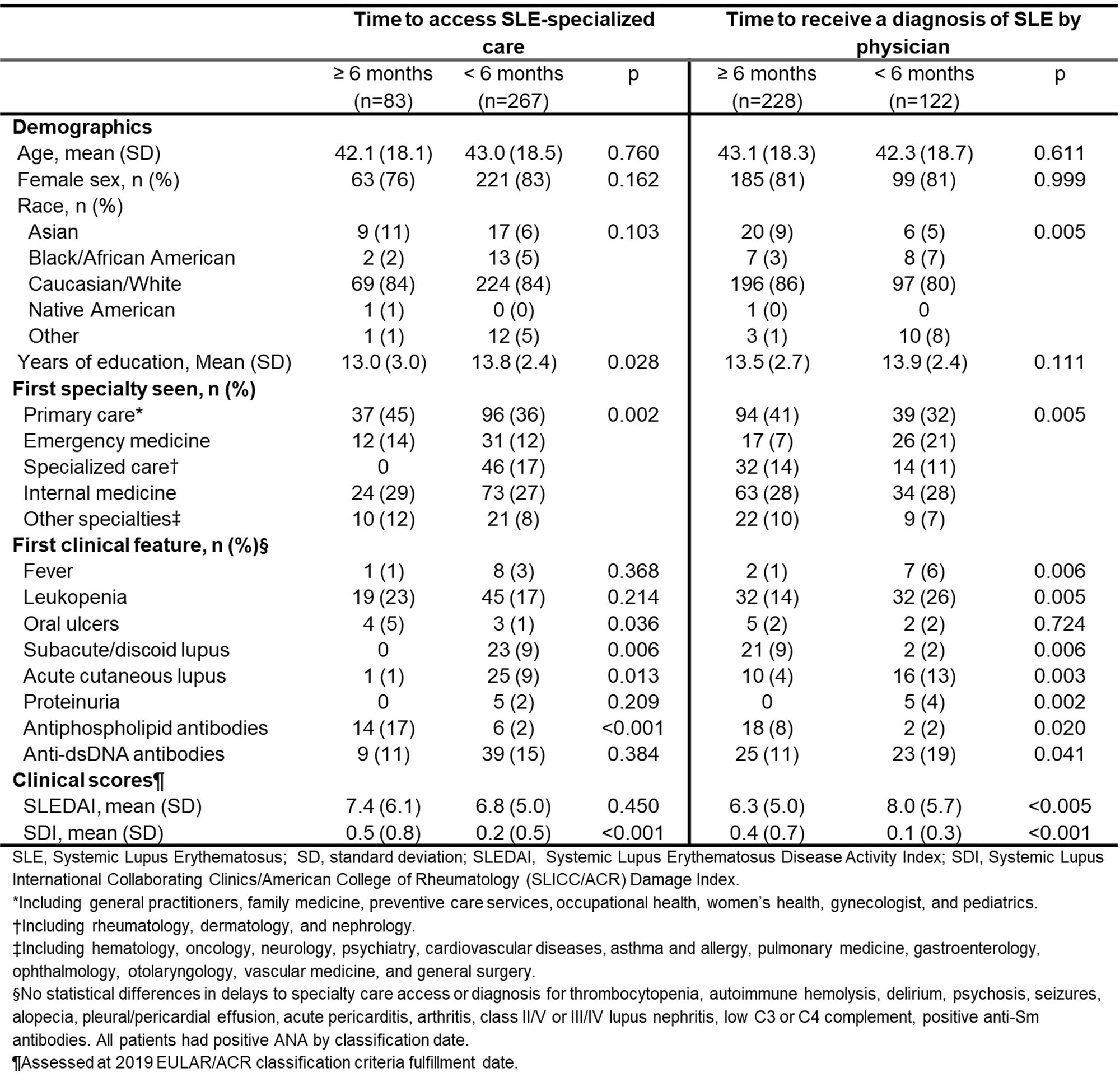
Results: A total of 350 incident SLE patients were included. Mean age (SD) was 42.8 years (18.4), and 81% were female. The majority of the patients were non-Hispanic White (84%). To access SLE-specialized care, median intervals from the first clinical contact were 1.6 months (IQR 0.3-14), and 3 clinical encounters (IQR 2-4) with 32% delays in access. Patients with delays in access had fewer years of education 13.0 (SD 3.0) vs.13.8 (SD 2.4), (p=0.028), oral ulcers (p=0.0036) and positive antiphospholipid antibodies (aPL) as first feature (p< 0.001) and higher damage score [mean SDI 0.5 (SD 0.8) vs. 0.2 (SD 0.4), (p< 0.01)]. The median time from first clinical contact to diagnosis was 8.3 months (IQR 1.4-58.2). Before receiving a diagnosis, patients needed a median of 2 specialties (IQR1-4), and 6 clinical encounters (IQR 3-13), with 65% having delays. Diagnostic delays were more frequent in Asians (p=0.005) and were less likely to debut with symptoms of abrupt onset (e.g., fever and malar rash) but had more cases of subacute/discoid lupus (p=0.006) and positive aPL (p=0.016) during first contact. Patients first assessed by primary care specialties had delays in diagnosis more frequently compared to those seen first by emergency medicine (p=0.005). This group also had lower disease activity [mean SLEDAI 6.3 (SD 5.0) vs 8.0 (SD 5.6), (p< 0.01)] but higher damage scores [mean SDI 0.4 (SD 0.6) vs. 0.1 (SD 0.2), (p< 0.01)] than those with early diagnosis. (Table 1)
Conclusion: One out of 3 patients had delayed access to specialized care, and two in three had delays in diagnosis. Delays were associated with disparities in race and education, but also with specific features during first contact and increased damage at classification date. Targeted efforts to improve early recognition and referral may prevent irreversible damage and improve the long-term prognosis of SLE.
To cite this abstract in AMA style:
Sanchez-Rodriguez A, Meade-Aguilar J, Yang J, Figueroa Parra G, Osei-Onomah S, Giblon R, Langenfeld H, Chamberlain A, Crowson C, Duarte-Garcia A. Delays in Access to Specialized Care and Diagnosis in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/delays-in-access-to-specialized-care-and-diagnosis-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/delays-in-access-to-specialized-care-and-diagnosis-in-patients-with-systemic-lupus-erythematosus/