Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Pulmonary arterial hypertension (PAH) is a leading cause of death in SLE patients. Hypocomplementemia, antiphospholipid antibodies, and elevated antibodies to RNP and Ro are correlated with SLE-associated PAH. In this study, we sought to define the SLE phenotype associated with PAH.
Methods: 207 (8%) SLE patients with pulmonary hypertension (PH), defined as a right ventricular systolic pressure greater than 40 mmHg on transthoracic echocardiogram or as pulmonary artery dilatation noted on CT of the chest, were identified from a longitudinal SLE cohort (94% female, 56.5% African American, 39% Caucasian, mean age 45.6 years). All patients with SLE met either the revised ACR or SLICC classification criteria.
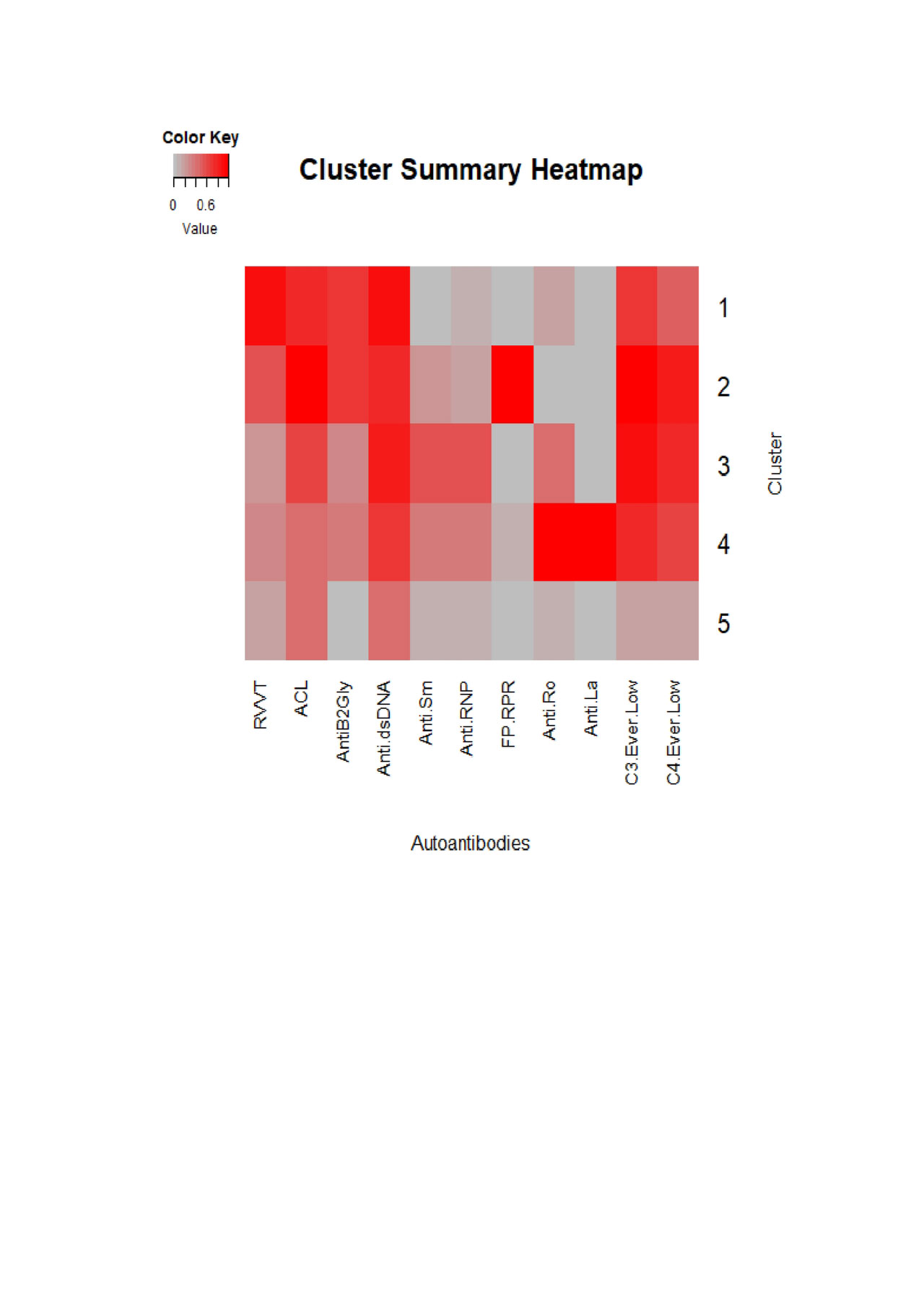
136 patients with SLE and PAH were eligible for the cluster analysis, as they had information available for all 11 selected autoantibodies (lupus anticoagulant, anticardiolipin, anti-beta2 glycoprotein 1, anti‐dsDNA, anti‐Sm, anti‐RNP, false positive(FP)‐RPR, anti‐Ro, anti‐La, and hypocomplementemia (C3 ever low or C4 ever low)). Agglomerative hierarchical clustering algorithm with Ward’s method was used to cluster the patients who had PAH, based on their history of autoantibodies. All analyses were performed in JMP version 13.0 and R version 3.5.1 using package cluster and gplots.
Results: Five clusters were identified, representing five different phenotypes. Clusters 1 and 2 had high frequencies of hypocomplementemia, antiphospholipid antibodies, and anti-dsDNA. Cluster 2 additionally had a high frequency of FP-RPR. Cluster 3 had high frequencies of hypocomplementemia, anticardiolipin, anti-Sm, anti-RNP, and anti-dsDNA, but only moderate frequencies of anti-Ro. Cluster 4 had high frequencies of hypocomplementemia, anti-Ro, anti-La, and anti-dsDNA. Cluster 5 had only moderate frequencies of anti-dsDNA and anticardiolipin.
Conclusion: Our data indicate an important association in several, but not all, clusters between antiphospholipid and PAH in SLE. Elevated anti-dsDNA and hypocomplementemia in some clusters may represent an association with active SLE in these subsets. Two clusters were antiphospholipid antibody predominant and two clusters were extractable nuclear antigen predominant, which may represent different pathophysiology and associate with divergent responses to immunosuppressive therapy.
To cite this abstract in AMA style:
Mizus M, Li J, Goldman D, Petri M. Defining the SLE-Associated Pulmonary Arterial Hypertension Phenotype [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/defining-the-sle-associated-pulmonary-arterial-hypertension-phenotype/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/defining-the-sle-associated-pulmonary-arterial-hypertension-phenotype/