Session Information
Date: Monday, November 18, 2024
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders II
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Lack of awareness and disease heterogeneity are common factors associated with diagnosis delay in patients with Relapsing polychondriytis (RP). Using latent class analysis (LCA), phenotypic subgroups have been identified in a prospective cohort of patients with RP. Identifying these subgroups can help clinicians to recognize patterns of organ involvement, facilitating prompt diagnosis.This study aimed to validate previously identified clinical subgroups using LCA and develop a decision tree algorithm to accurately predict assignment of individual patients to these subgroups.
Methods: Patients ≥ 18 years old who met diagnostic criteria for RP were included. All patients had a dynamic chest computerized tomography (CT) and audiometry. LCA was conducted in two independent prospective cohorts of patients with RP using the following variables: arthritis, tracheomalacia, bronchomalacia, subglottic stenosis, ear damage, nose damage, eye inflammation, and sensorineural hearing loss. Ear damage was defined by thickening of the cartilage or cauliflower ear. Nose damage was defined by saddle nose deformity or nasal septal perforation. Tracheomalacia and bronchomalacia were defined as ≥ 50% airway collapse on dynamic chest CT. Optimization of latent class models was performed using Bayesian information criterion (BIC) and Akaike information criterion (AIC). Decision tree analysis was performed to predict latent class group status.
Results: 162 patients with RP were included in this study. Cohort #1 included 102 patients: 92 (90%) females; 93 (91%) Caucasians; median age 48 years (IQR= 38-59). Cohort #2 included 60 patients: 52 (86%) females; 52 (86 %) Caucasians; median age 44 years (IQR=38-52).
Three clinical subgroups were identified by LCA in each cohort: Type 1 was characterized by ear damage, nose damage and subglottic stenosis, Type 2 was characterized by tracheomalacia and bronchomalacia, and Type 3 was characterized by absence of tracheomalacia.
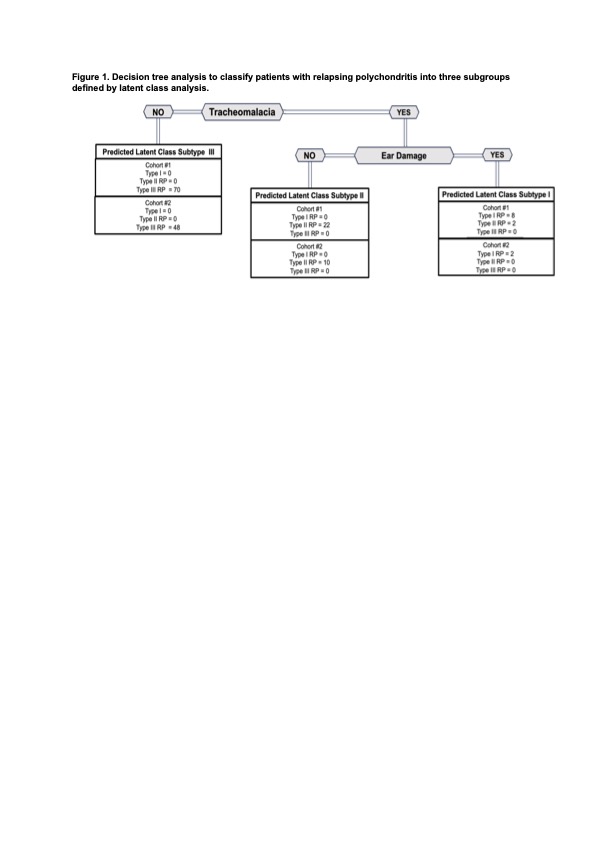
Tracheomalacia and ear damage were the two critical variables found on the decision tree that predicted latent class assignment in both cohorts. In cohort #1, the accuracy was 98% (R-square = 0.91) and in cohort #2 the accuracy was 100% (R-square=0.95) (Figure 1).
Figure 1
Figure 1. Decision tree analysis to classify patients with relapsing polychondritis into three subgroups defined by latent class analysis.
Conclusion: This study corroborates the existence of previously identified clinical subtypes of RP. Tracheomalacia and ear damage effectively categorize patients into these subgroups. These findings support the potential use of this subgrouping in clinical practice and clinical research design.
To cite this abstract in AMA style:
Banerjee S, McAlear C, Merkel P, Grayson P, Ferrada M. Defining Clinical Subgroups of Patients with Relapsing Polychondritis: A Latent Class and Decision Tree Analysis in Two Independent Prospective Cohorts [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/defining-clinical-subgroups-of-patients-with-relapsing-polychondritis-a-latent-class-and-decision-tree-analysis-in-two-independent-prospective-cohorts/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/defining-clinical-subgroups-of-patients-with-relapsing-polychondritis-a-latent-class-and-decision-tree-analysis-in-two-independent-prospective-cohorts/