Session Information
Date: Monday, November 9, 2015
Title: Imaging of Rheumatic Diseases Poster II: X-ray, MRI, PET and CT
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Imaging-detected inflammation persists in many rheumatoid arthritis (RA) patients
despite therapy. We used data from two clinical trials of golimumab to
determine thresholds for RA magnetic resonance imaging scores (RAMRIS) for synovitis
and osteitis associated with a low risk of radiographic and MRI progression in
structural damage.
Methods: MRI of the dominant hand was performed and RAMRIS scores were determined
at weeks 0, 24, and 52. X-rays were also performed and van der Heijde-Sharp
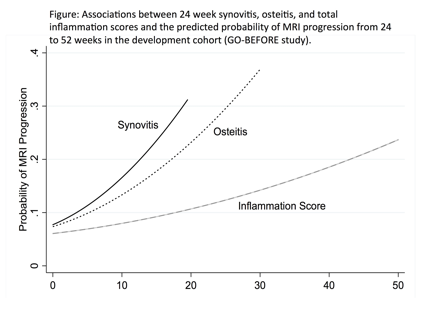
scores (vdHS) determined. .In a development cohort (GO-BEFORE) the changes in
MRI erosion score and vdHS score were determined over the 24-week to 52-week
interval. MRI erosion and vdHS progression were defined as a change of >0.5.
We aimed to identify 24-week thresholds for synovitis (total possible score 21)
and osteitis (possible score 230) that provided approximately 90% sensitivity
for MRI erosion progression over the 24 to 52 week interval. Rates of
progression were illustrated over the range of synovitis, osteitis, and a
combination (total inflammation score) at the beginning of the interval. The
performance of the cutoffs was then tested in a validation cohort (GO-FORWARD).
Results: In
the development cohort, subjects who reached a synovitis or osteitis score
<=5 by 24 weeks had a low probability of progression on MRI and X-ray
between 24 and 52 weeks (8% and 9%, respectively). The coefficient for osteitis
was stronger than that of synovitis in multivariable models predicting X-ray
and MRI progression. Therefore, when these scores were combined into a single
inflammation score, the score was weighted on osteitis (x2). In the validation
cohort, subjects who reached an inflammation score of <=10 by 24 weeks had a
low predicted probability of progression from 24 to 52 weeks (7%). In the
validation cohort, there was a low rate of MRI progression between 24 and 52
weeks among those with low synovitis, osteitis, and inflammation scores (Table)
independent of 24-week DAS28 or C-reactive protein. A lower risk of x-ray
progression was observed between 0 and 52 weeks among 34% of subjects with a
low inflammation score at baseline as well as among the 47% and 49% of subjects
who reached a low inflammation score by weeks 12 or 24, respectively.
Conclusion:
Patients that reach low
levels of MRI inflammation by 3 or 6 months are substantially less likely to
have structural damage progression independent of DAS28 response. A low score
by 6 months is predictive of a low risk of radiographic progression over 52
weeks, suggesting that these outcomes might potentially be used as early
dichotomous endpoints in clinical studies.
To cite this abstract in AMA style:
Baker J, Østergaard M, Baker D, Emery P, Conaghan PG. Defining an Acceptable Level of MRI Inflammation in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/defining-an-acceptable-level-of-mri-inflammation-in-rheumatoid-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/defining-an-acceptable-level-of-mri-inflammation-in-rheumatoid-arthritis/