Session Information
Date: Sunday, November 8, 2020
Title: Epidemiology & Public Health Poster III: Inflammatory Rheumatic Disease
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus is a serious, multi-system autoimmune disease that affects young people. Mortality is increased by over 2-3 fold compared to the general population. Time-trends showed a reduction in mortality in a multicentric lupus cohort from 1970 to 2001 and in a U.S. population-based lupus cohort from 1950 to 1992. In contrast, in a study using the U.S. National center for Health Statistics and National Inpatient Sample (NIS) data, in-hospital mortality was 2.9% and it increased from 1978 to 1998. Given these contradictory time-trends and the lack of contemporary data in lupus, an updated study of mortality are needed. Our objective was to assess the time-trends in in-hospital mortality rates in people with lupus hospitalized in the U.S. from 1998 to 2014, and compare it to people without lupus.
Methods: We included discharges from the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS) for 1998 through 2014, the last year of the use of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The NIS is a 20% stratified sample of hospital discharges which is designed for creating national estimates.
We identified primary lupus hospitalizations based on the presence of an ICD-9-CM code of 710.0x in the primary position; this diagnostic code approach has a sensitivity of 98% and specificity of 72%.
We calculated the unadjusted in-hospital mortality rates per 1,000 hospitalizations for people with versus without primary lupus hospitalizations, with the respective denominators. Rates were adjusted by age, grouped in quintiles (< 20, 20-39, 40-59, 60-79, >79) then by age and sex. We analyzed for time-trends in rates over time using Cochran Armitage test, weighted by the number of hospitalizations in each year.
Results: The 241,130 primary lupus hospitalizations in 1998-2014 included predominantly black (34.3%), young (45% were 20-39 years; mean age, 36 years) and female (86.9%) patients. Deyo-Charlson comorbidity score was ≥2 for 47%, approximately 1/3rd were receiving Medicaid and 1.5% died during the index hospitalization (Table 1).
Unadjusted mortality in primary lupus hospitalizations decreased by 45.2% from 17.9 in 1998 to 9.5 per 1,000 in 2014, versus a 25.9% reduction in non-lupus (28.1 to 21.2 per 1,000; Figure 1). Age and sex-adjusted mortality gap by lupus also decreased: primary lupus hospitalization, 17.6 per 1,000 claims in 1998 to 13.8 in 2014 (21.5% reduction), versus 15.1 per 1,000 claims in 1998 to 13.2 in 2014 in non-lupus (12.5% reduction; Figure 1; Table 2). This caused the line of mortality rates for those with primary lupus hospitalization to overlap with that of the rest of the population. The number of primary lupus hospitalizations remained fairly constant at 12-15,000 per year 1998-2014 (i.e., 0.04% of all NIS claims), and the rate per 100,000 NIS claims was 40.3 in 1998-2000 versus 34.9 in 2013-2014; the annual rates of total NIS hospitalizations were also stable 1998-2014.
The lupus to non-lupus mortality rate ratio was 1.17 in 1998 and 1.04 in 2014.
Conclusion: The reduction in in-hospital mortality in people with lupus exceeded than in non-lupus, including age-and sex-adjusted. The improved in-hospital mortality in lupus is encouraging.
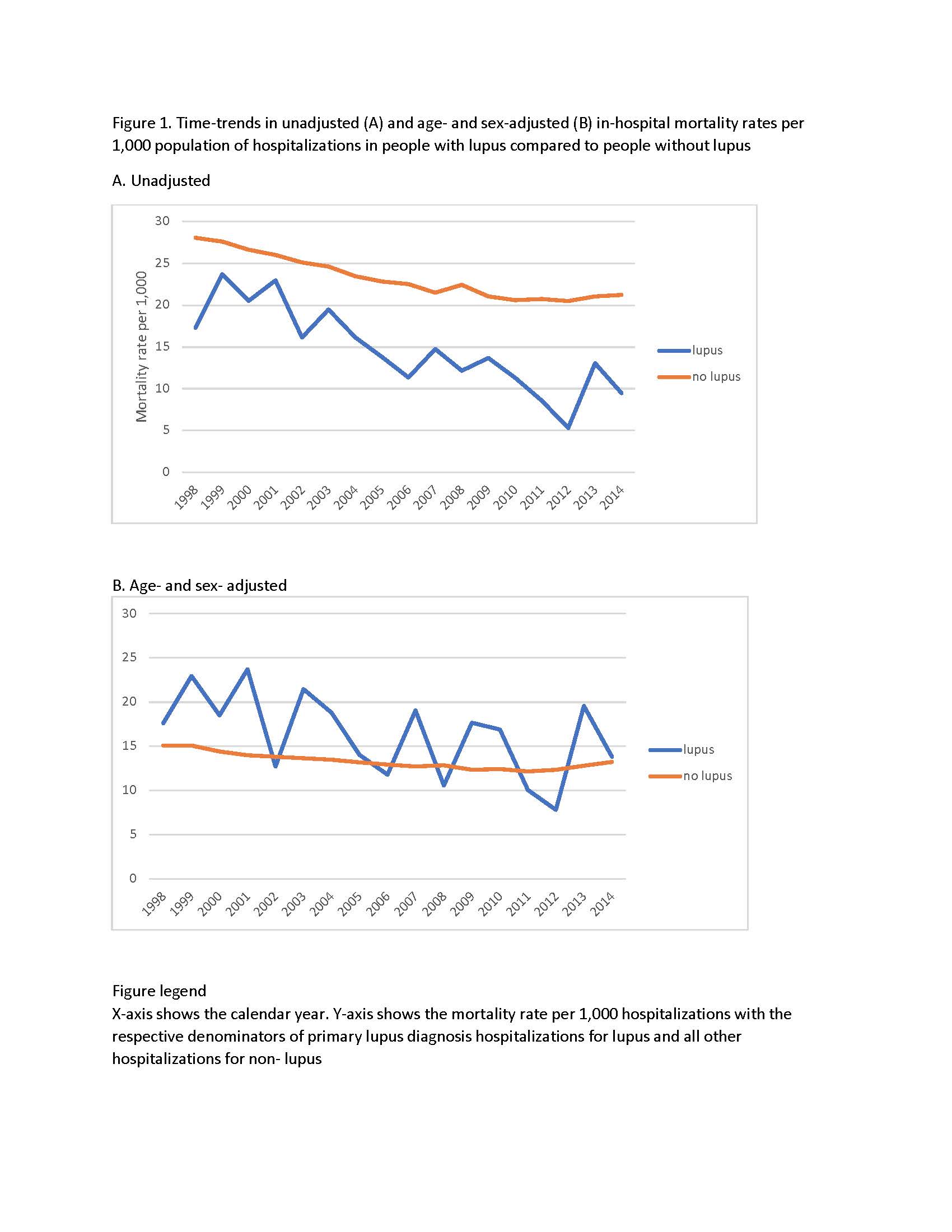 Figure 1. Time-trends in unadjusted (A) and age- and sex-adjusted (B) in-hospital mortality rates per 1,000 population of hospitalizations in people with lupus compared to people without lupus A. Unadjusted B. Age- and sex- adjusted Figure legend X-axis shows the calendar year. Y-axis shows the mortality rate per 1,000 hospitalizations with the respective denominators of primary lupus diagnosis hospitalizations for lupus and all other hospitalizations for non- lupus
Figure 1. Time-trends in unadjusted (A) and age- and sex-adjusted (B) in-hospital mortality rates per 1,000 population of hospitalizations in people with lupus compared to people without lupus A. Unadjusted B. Age- and sex- adjusted Figure legend X-axis shows the calendar year. Y-axis shows the mortality rate per 1,000 hospitalizations with the respective denominators of primary lupus diagnosis hospitalizations for lupus and all other hospitalizations for non- lupus
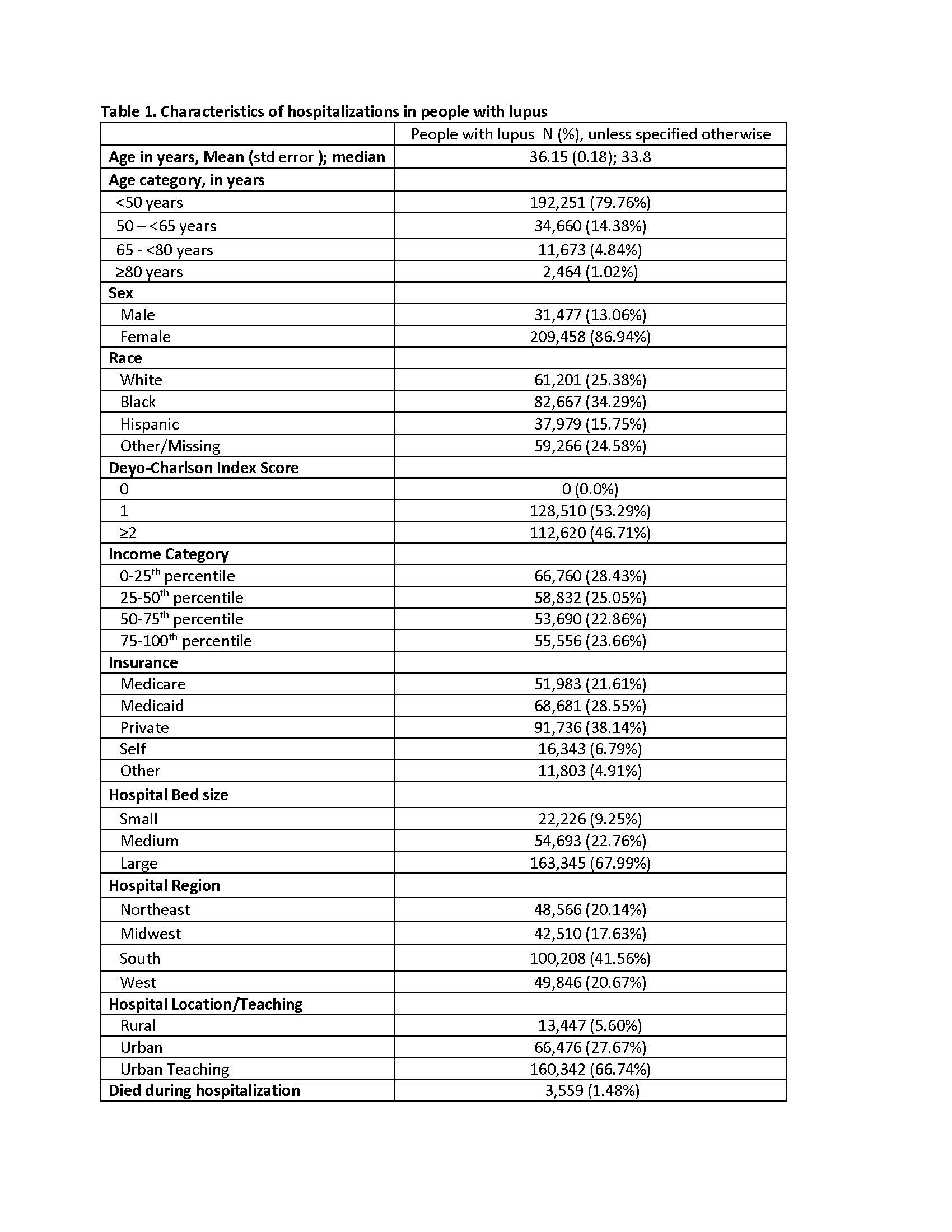 Table 1. Characteristics of hospitalizations in people with lupus
Table 1. Characteristics of hospitalizations in people with lupus
 Table 2. Comparison of Mortality rates per 1,000 hospitalized people between lupus vs. non-lupus: unadjusted based on the NIS sample; age- and age- and sex-adjusted rates based on the NIS sample and the census data
Table 2. Comparison of Mortality rates per 1,000 hospitalized people between lupus vs. non-lupus: unadjusted based on the NIS sample; age- and age- and sex-adjusted rates based on the NIS sample and the census data
To cite this abstract in AMA style:
Singh J, Cleveland J. Declining In-hospital Mortality Gap in Lupus Compared to Non-lupus Hospitalizations: A National Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/declining-in-hospital-mortality-gap-in-lupus-compared-to-non-lupus-hospitalizations-a-national-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/declining-in-hospital-mortality-gap-in-lupus-compared-to-non-lupus-hospitalizations-a-national-study/
