Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: The advent of biologic medications, such as subcutaneous TNF-alpha inhibitors (SC-TNFi), has transformed the management of inflammatory arthritis (IA) during the last decades. However, a significant proportion of patients with IA fail to respond, lose response, or experience adverse events while being treated with a biologic, and may therefore be required to discontinue or switch treatment. The aim of this study was to identify IA patient subgroups with different levels of treatment persistence through decision tree analysis using recursive partitioning methods.
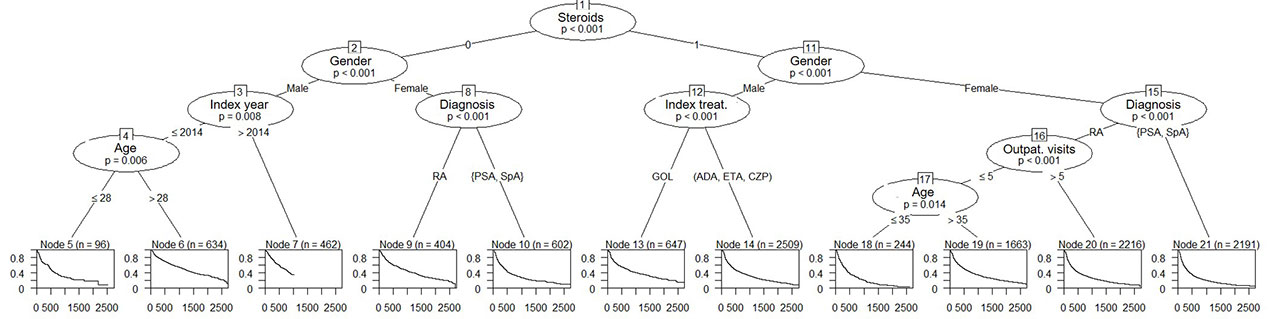
Methods: Using data from Swedish Health Data Registers, adult, biologic treatment-naïve patients initiating treatment for IA with any available SC-TNFi (adalimumab, etanercept, certolizumab, and golimumab) between May 1, 2010 and October 31, 2016 were included. Treatment persistence was derived based on information from filled prescriptions (e.g. dispensing date, pack information, and defined daily dose) and a grace period of 60 days. A number of covariates were derived from data collected in the year prior to treatment initiation, including Charlson Comorbidity Index and its components, number of visits and inpatient stays in specialized care, and treatment initiation year, and filled prescriptions for systemic corticosteroids, DMARDs and/or NSAIDs. In addition, age at treatment initiation, sex, IA diagnosis [spondyloarthritis (SpA) / psoriatic arthritis (PsA) / rheumatoid arthritis (RA)], index biologic treatment were included as covariates in the analysis. The decision tree was created through recursive partitioning, and the analysis was performed with the cTree method (in R statistical software), which uses a conditional inference framework. Differences between terminal nodes were examined using log-rank tests.
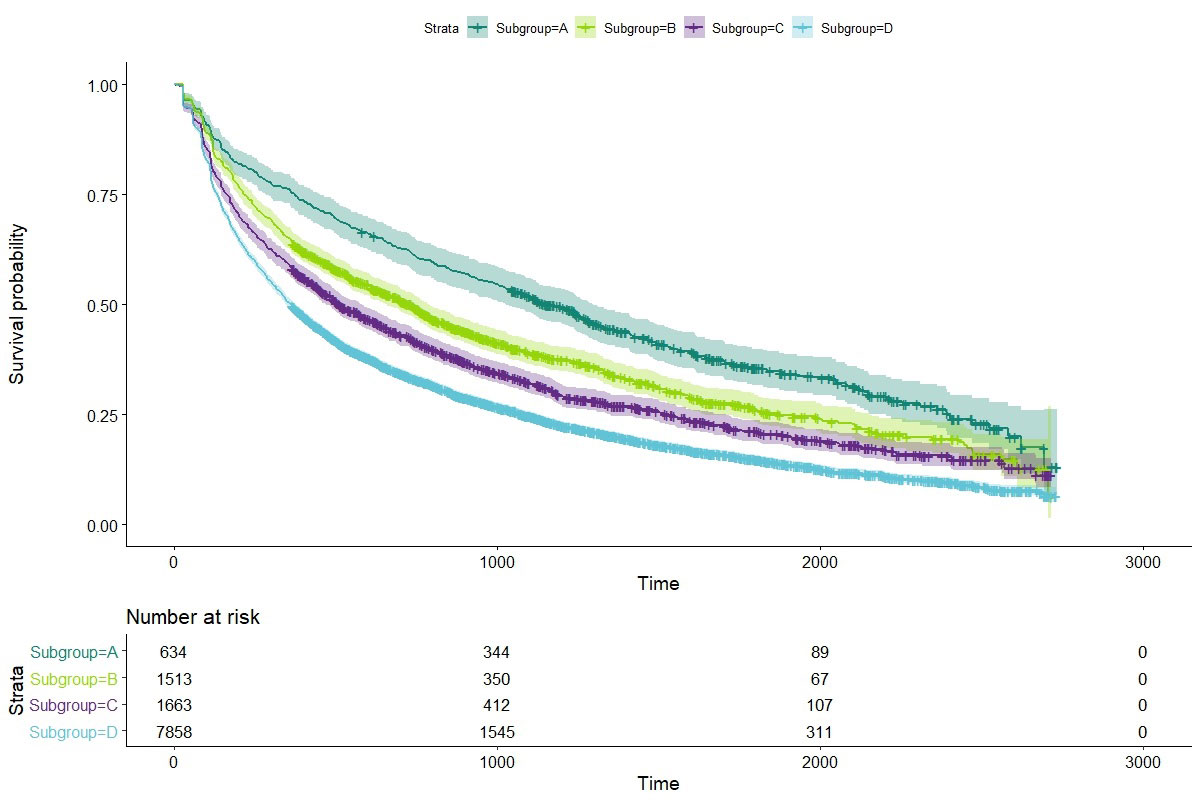
Results: A total of 11,668 patients were included in the study. The decision tree analysis resulted in 11 terminal nodes (Figure 1). The highest persistence was found in male patients, aged over 28 years who did not use systemic corticosteroids in the year prior to SC-TNFi initiation, and who initiated treatment prior to 2015. The lowest persistence was found in females with a diagnosis of SpA or PsA using systemic corticosteroids in the year prior to treatment initiation. Four groups of patients were found to have significant differences in drug persistence when the terminal node subgroups were compared. Median survival by group ranged between 1 year and 3.2 years (Figure 2). Golimumab was the only therapy that has a positive predictive effect on persistence.
Conclusion: This study uses a conditional inference method for decision tree analysis to identify patient subgroups with different levels of treatment persistence. The results may serve as a basis for further research needed to understand the reasons for treatment discontinuation in subgroups with low drug persistence. In addition, the results from this analysis may aid physicians in anticipating treatment persistence and monitor certain subgroups of patients more closely who are more likely to discontinue treatment.
To cite this abstract in AMA style:
Hernlund E, Klint J, Svedbom A, Dalén J, Black C, Puenpatom A. Decision Tree Analysis to Identify Inflammatory Arthritis Patient Subgroups with Different Levels of Treatment Persistence with First-Line Subcutaneous TNF-alpha Inhibitors [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/decision-tree-analysis-to-identify-inflammatory-arthritis-patient-subgroups-with-different-levels-of-treatment-persistence-with-first-line-subcutaneous-tnf-alpha-inhibitors/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/decision-tree-analysis-to-identify-inflammatory-arthritis-patient-subgroups-with-different-levels-of-treatment-persistence-with-first-line-subcutaneous-tnf-alpha-inhibitors/