Session Information
Date: Sunday, November 7, 2021
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: The ASAS definition of a positive MRI for inflammation in the spine (ASAS-MRI+) is intended for classification of patients as having axSpA but is often misused for diagnostic purposes. This is problematic because bone marrow edema (BME) in the spine may occur in 20-40% of both healthy individuals as well as those with mechanical back disorders. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the spine. These definitions have been validated by 8 readers from the ASAS-MRI group on MRI spine images from the ASAS Classification Cohort. We aimed to identify quantitative cut-offs based on numbers of vertebral corners that define a positive MRI for axSpA, there being two gold standards: A. majority central reader decision as to the presence of spine MRI findings consistent with axSpA B. rheumatologist expert opinion diagnosis of axSpA
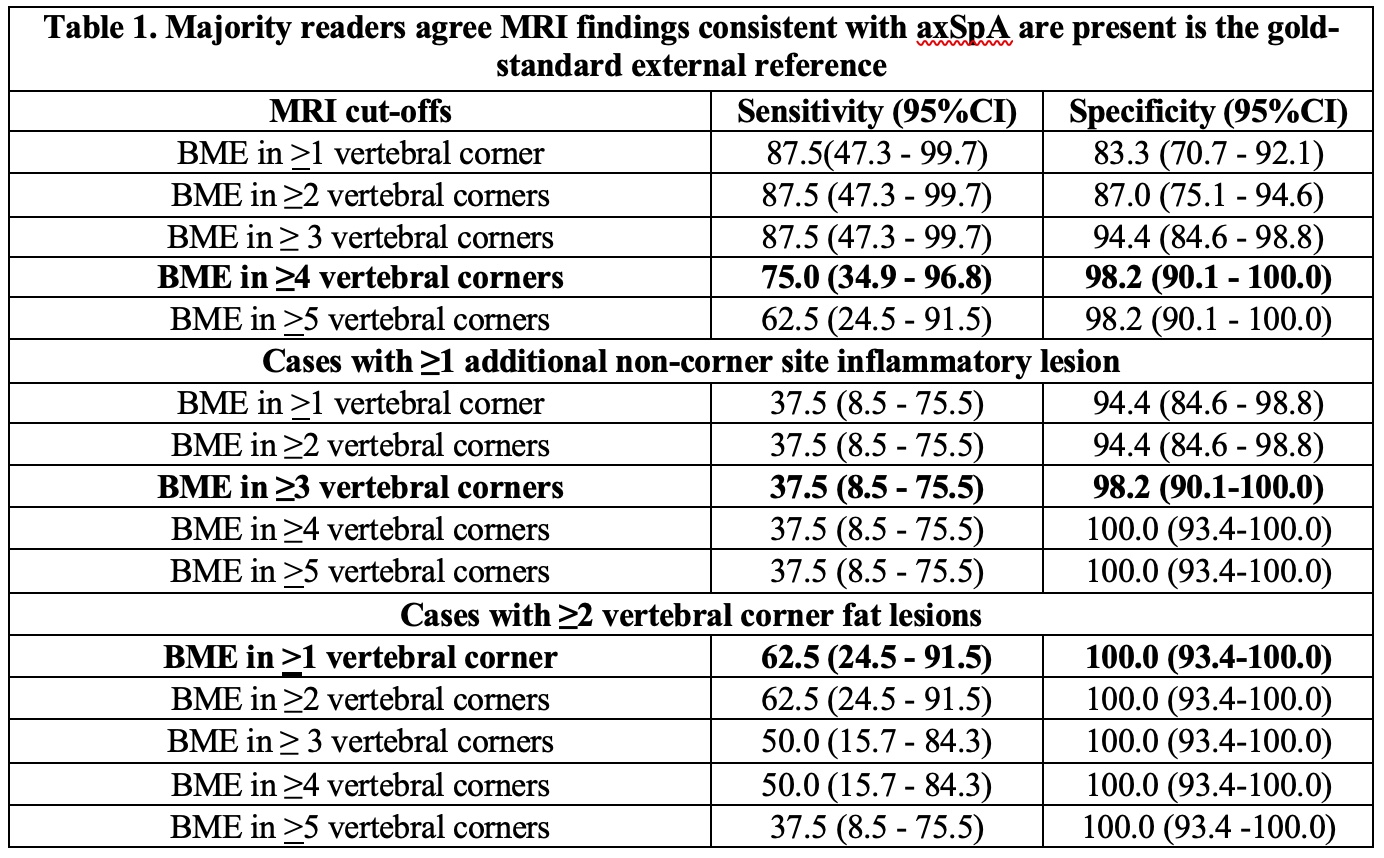
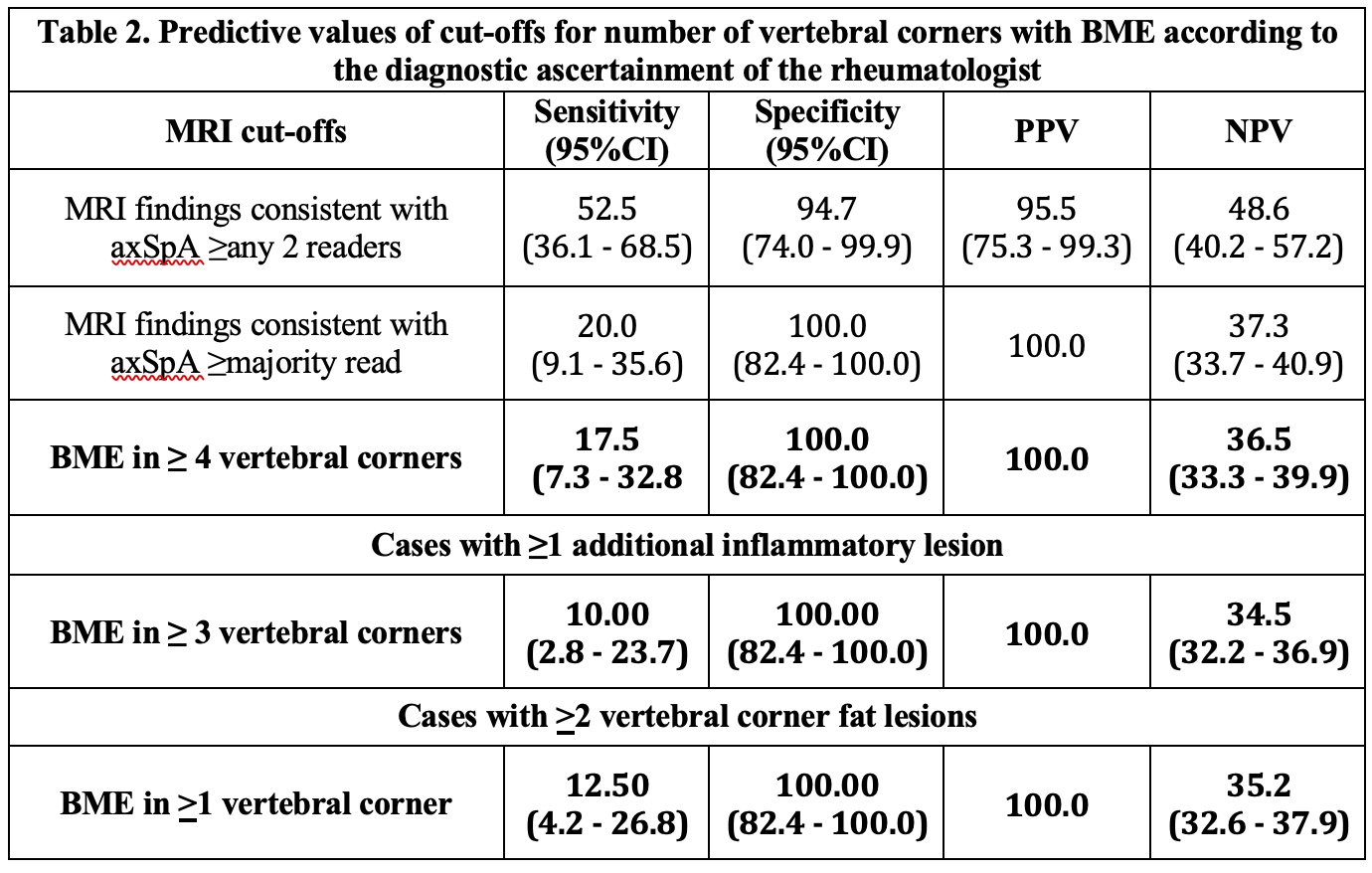
Methods: Eight ASAS-MRI readers recorded MRI lesions in the spine of 62 cases recruited to the ASAS classification cohort according to recently updated ASAS definitions in an eCRF that comprises global assessment (are the findings on this MRI scan consistent with axSpA? (yes/no)), and detailed scoring of lesions for all sites in the spine, including vertebral bodies, lateral and posterior elements. We calculated sensitivity and specificity for numbers of vertebral corners with BME (VC-BME) where a majority of readers (>5/8) agreed as to the presence of MRI findings consistent with axSpA. We selected optimal cut-offs with ≥95% specificity. These cut-offs were analyzed for their predictive utility for rheumatologist diagnosis of axSpA by calculating positive and negative predictive values (PPV, NPV) and selecting those cut-offs with PPV of ≥95%. Both specificity of ≥95% for MRI consistent with axSpA as well as a PPV of ≥95% for rheumatologist diagnosis were considered requirements for preliminary designation of MRI cut-offs defining a positive spine MRI consistent with axSpA.
Results: MRI findings consistent with axSpA were observed in the spine by majority read in 8 (20%) of 40 cases diagnosed with axSpA, and 0 (0%) of 19 cases without axSpA. Cut-offs achieving specificity of ≥95% for MRI findings consistent with axSpA were 4 VC-BME (sensitivity 75%) for all cases, 3 VC-BME (sensitivity 37.5%) for cases with ≥1 additional location with inflammation, 1 VC-BME (sensitivity 62.5%) in cases with >2 vertebral corner fat lesions (Table 1). All of the above cut-offs also had very high positive predictive values (≥95%) for diagnosis of axSpA in cases diagnosed by the rheumatologist (Table 2).
Conclusion: A cut-off of BME in ≥4 vertebral corners, or ≥3 corners in the setting of additional inflammatory lesions at other locations or corner fat, are primary candidates for defining a positive MRI of the spine consistent with axSpA. The PPV performance of these MRI cut-offs for rheumatologist diagnosis of axSpA apply to typical patients referred to a rheumatologist with a high index of suspicion of axSpA and may not be appropriate in other populations.
To cite this abstract in AMA style:
Maksymowych W, Lambert R, Baraliakos X, Pedersen S, Eshed I, Weber U, Machado P, de Hooge M, Sieper J, Wichuk S, Poddubnyy D, Rudwaleit M, Landewé R, van der Heijde D, Ostergaard M. Data-driven Definitions Based on Inflammatory Lesions for a Positive MRI of the Spine Consistent with Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/data-driven-definitions-based-on-inflammatory-lesions-for-a-positive-mri-of-the-spine-consistent-with-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/data-driven-definitions-based-on-inflammatory-lesions-for-a-positive-mri-of-the-spine-consistent-with-axial-spondyloarthritis/