Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Multiple joint osteoarthritis (MJOA) may represent a unique phenotype of osteoarthritis related to systemic factors associated with pathologic aging. We tested the hypothesis that metabolic syndrome and its components, frailty and its components and lower levels of bone density are associated with MJOA.
Methods: Participants in the Osteoarthritis Initiative (N=3325) had hand, hip and knee xrays performed and centrally read for osteoarthritis. Hand osteoarthritis (OA) was defined as at least one joint with Kellegren-Lawrence(KL) >2 on at least two rays; Hip OA was defined as modified Croft grade >2 in ether hip; Knee OA was defined as KL >2 in either knee. MJOA was defined as hand OA and either hip or knee OA. A metabolic syndrome score was developed based upon the presence of hypertension, diabetes, lipid disorder, and increased waist circumference. Fraility was defined as one positive on the Song Frailty index and evaluating waking speed, chair stands and self-reported energy. Cortical thickness of metacarpal bones digits 2-4 and femoral bone density (FMD) in a smaller sub-sample based upon DEXA estimated the effect of bone mineral density (BMD). Prevalence ratios and 95% confidence intervals were estimated using poisson regression.
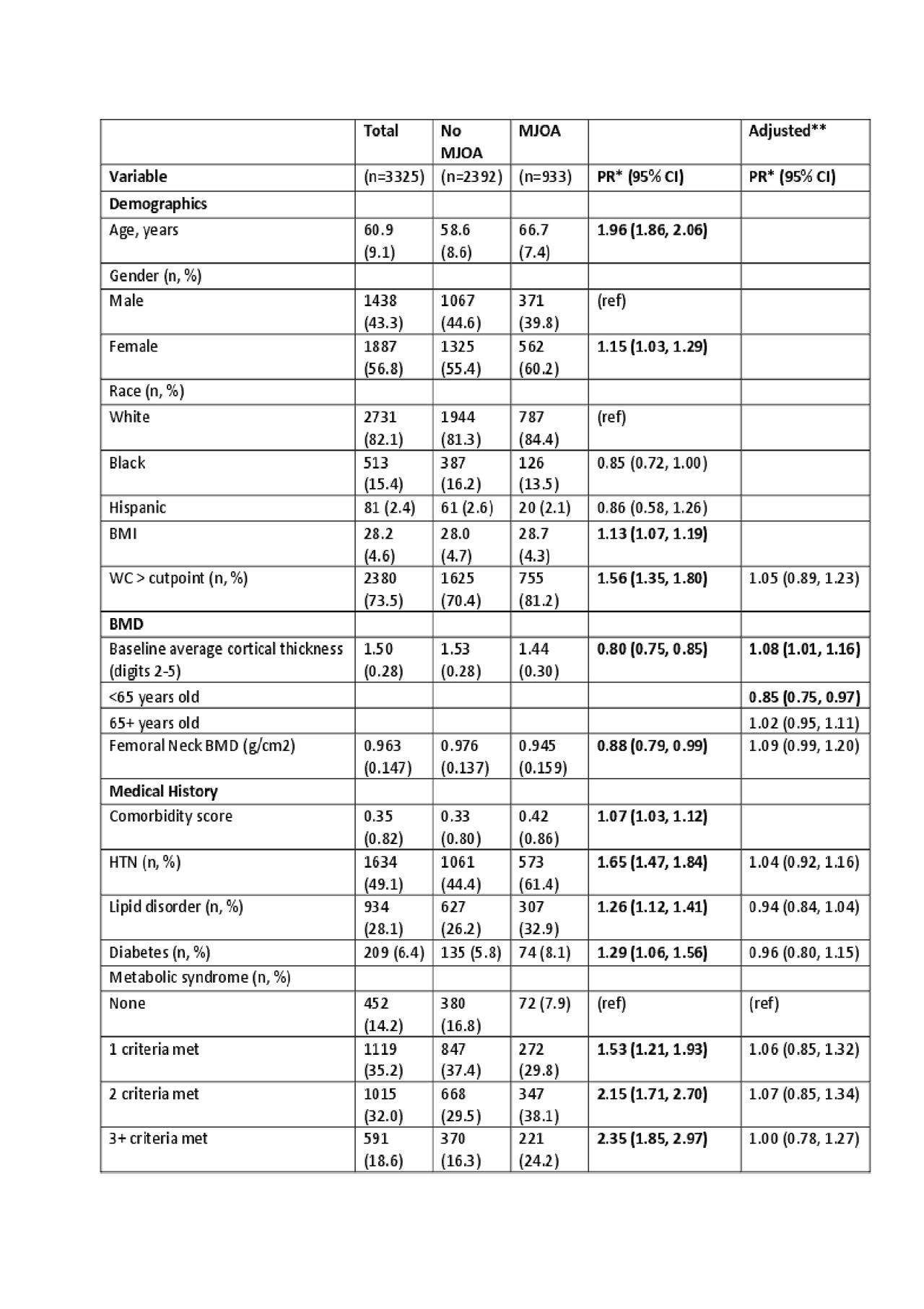
Results: Of the 3325 participants, 933 had MJOA and 2392 did not. The average age of the analytic cohort was 60.9 years, 56.8% were female, 82.1% were white, 15.4% were black and 2.4% were hispanic, and 11% had incomes < $25,000. Age, female gender, BMI, abdominal circumference, hypertension, lipid disorder, diabetes, metabolic syndrome score, Song Frailty index, slow walking speed, using hands during chair stands were associated with higher prevalence of MJOA. Higher levels of physical activity,bone mineral density, walking speed, chair stand pace, extensor and flexor strength of lower extremities were inversely associated with MJOA. In multiple variate analysis adjusting for age, gender, and BMI metabolic syndrome and its components were no longer associated with MJOA, thinner cortical thickness was only associated with MJOA in those < 65 years of age, and only slow walking speed as a measure of Frailty was associated with MJOA. Faster chair stand pace and dominant lower extremity extensor strength remained inversely associated with MJOA. ( See Table 1)
Conclusion: Age is a strongly associated with MJOA. Low bone density as measured by metacarpal cortical thickness at age less than 65, impaired walking speed, lower chair stand pace, decreased lower extremity extensor strength may reflect pathologic aging and are associated with MJOA in this cross-sectional analysis. Prospective analysis and exploring the underlying pathobiologic pathways associated with impaired BMD and muscle strength could lead to effective prevention and treatments of MJOA.
To cite this abstract in AMA style:
Eaton C, Roberts M, Driban J, Nevitt M, Duryea J, McAlindon T. Cross-sectional Associations of Multiple Joint Osteoarthritis in the Osteoarthritis Initiative [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/cross-sectional-associations-of-multiple-joint-osteoarthritis-in-the-osteoarthritis-initiative/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cross-sectional-associations-of-multiple-joint-osteoarthritis-in-the-osteoarthritis-initiative/