Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Early diagnosis for rheumatic conditions is crucial for children to achieve the best functional outcomes. Access to care is difficult due to the volume of referrals and paucity of pediatric rheumatologists. This compelling need to expediently triage dire and complex rheumatology referrals has been painfully demonstrated in our clinic. When this project was initiated there was a 3-month backlog to see a new referral. During this time, several patients were assigned delayed appointment dates due to our lack of a triage process. Improving the referral process so the appropriate patient is seen quickly is important for early diagnosis and earlier treatment, which improves quality of care for children with chronic debilitating rheumatic conditions. We intended to increase from 35% to 85% our rate of appointments scheduled within 30 business days for referred pediatric patients who require ongoing rheumatologic care by December 30, 2018. Our process measures were 0 to 90% increase in use of referral tool by primary care providers and 0 to 90% increase in appropriate use of triage tool by our clinic staff. Our balancing measures were no show rates and patient volume.
Methods: The improvement methodology used for this project was the Model for Improvement with rapid Plan, Do, Study, Act cycles. We defined current state by collecting baseline data, completing a root cause analysis, and surveying staff and patients to identify the most common and impactful barriers of lack of a standardized referral and triage process, lack of available appointments for higher acuity patients, and limitations in staff and families’ ability to make contact.
We used a Key Driver Diagram to define leading factors and guide change ideas, and an aim statement and data management plan to guide the work and data collection. Our measures were evaluated using run charts and later moved into a Statistical Process Control Chart.
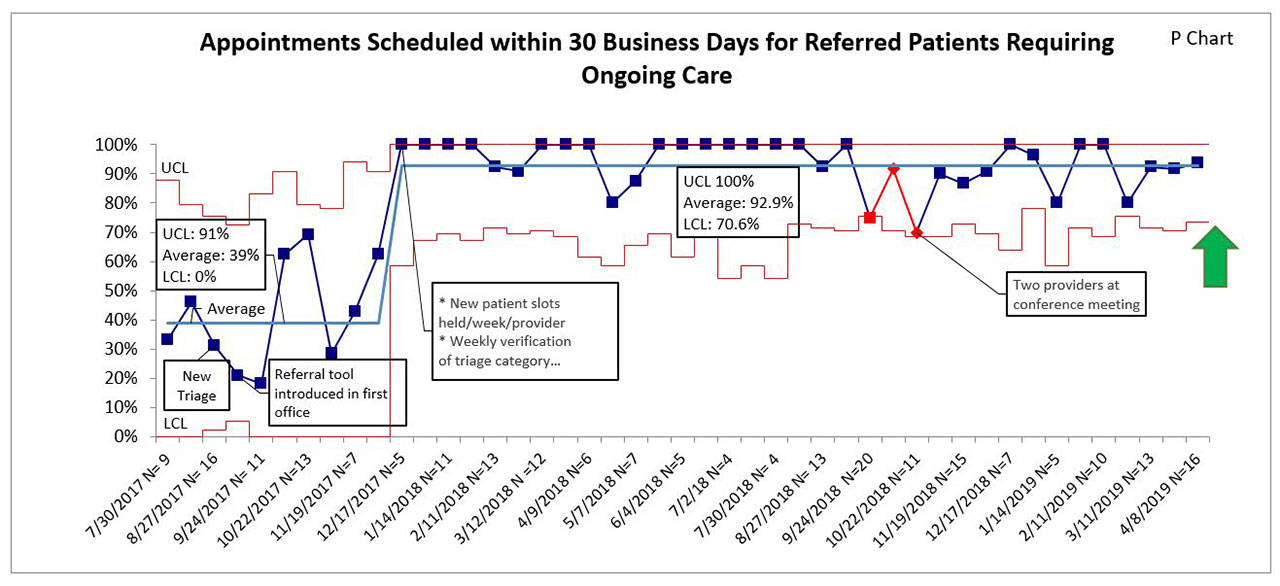
Results: We have sustained our average performance for our target population at 92% since December 2017 (Figure 1). This represents an 8% improvement over our initial goal of 85% and a 135% improvement over baseline.
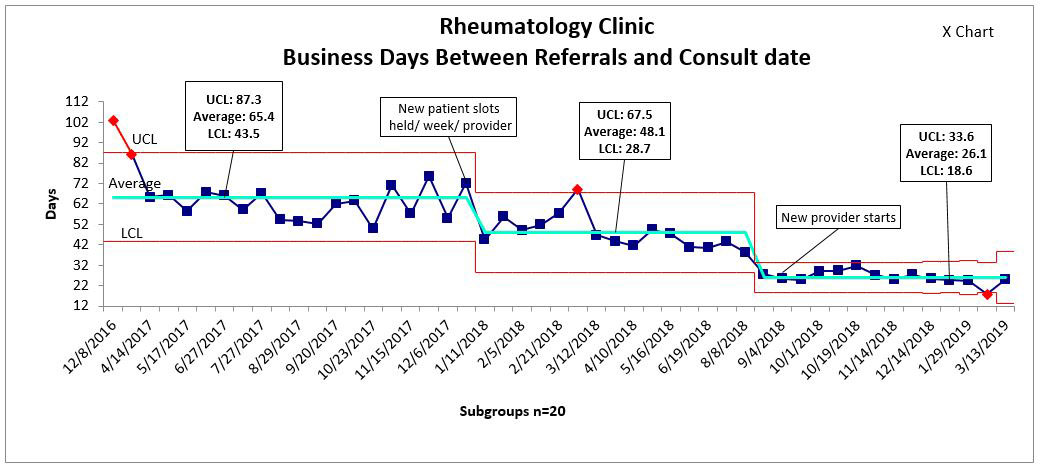
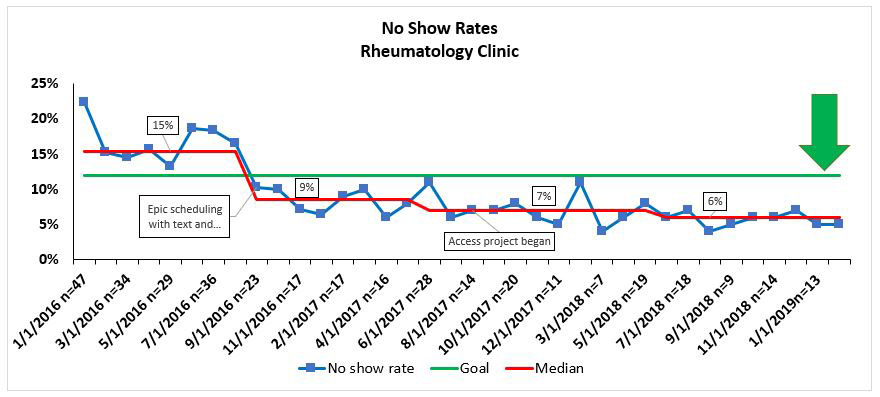
Additionally, we reduced time from referral received to the patient being seen by a provider for the overall clinic population from an average of 65.4 business days to 26.1 (Figure 2). Our no-show rate was reduced from 15% to 6% (Figure 3) and our total volume of patients increased by an average of 30 per month. This ultimately yielded a return on investment of greater than $300k in sixteen months.
Conclusion: Improvement science offers a methodology to strategically address inefficiencies and communication barriers, ensuring improved quality and safety, and better patient experience. By investing time in creative problem-solving, streamlining, and clear communication, and by facilitating staff empowerment and ownership, this project achieved remarkable gains in patient access and care delivery. Most importantly, we ensured longevity for this crucial improvement, thus promising significant long-term benefits. This result is a process that can be transferred to other settings, and holds great value given the universal challenges of supply/demand.
To cite this abstract in AMA style:
Vora S, Moyer A, Kalhagen L, Sherrod A, Griffin T, Corcoran K, Mabus S, Buitrago T. Cracks in Your Referral Process? Find Your Sustainable Solution Here [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/cracks-in-your-referral-process-find-your-sustainable-solution-here/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cracks-in-your-referral-process-find-your-sustainable-solution-here/