Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: People with immune mediated inflammatory diseases (IMIDs) are at greater risk of severe Coronavirus disease (COVID-19). Vaccination reduces COVID-19 severity however, vaccine uptake may be different for people with IMIDs versus the general population. We used provincial administrative health data from a province with a population of >1.3 million and universal health care coverage, including vaccines, to compare vaccine uptake and COVID-19 related hospitalization in people with diagnosed IMID versus the general population.
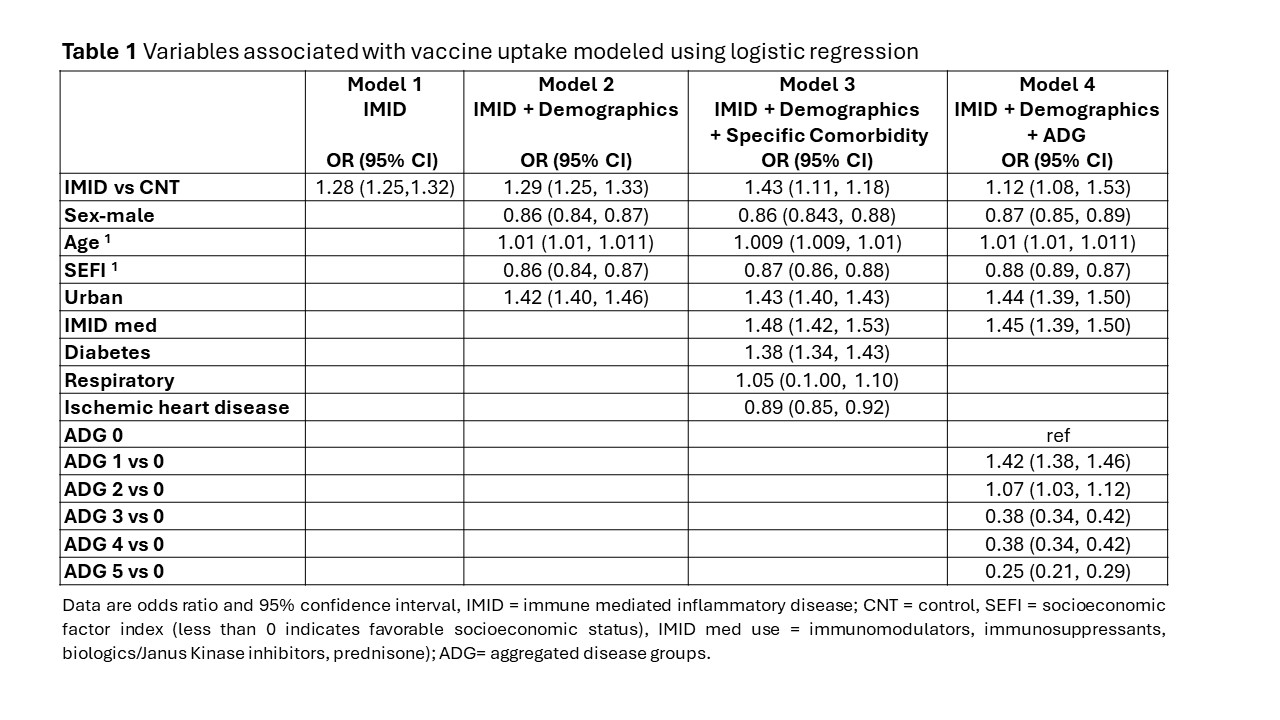
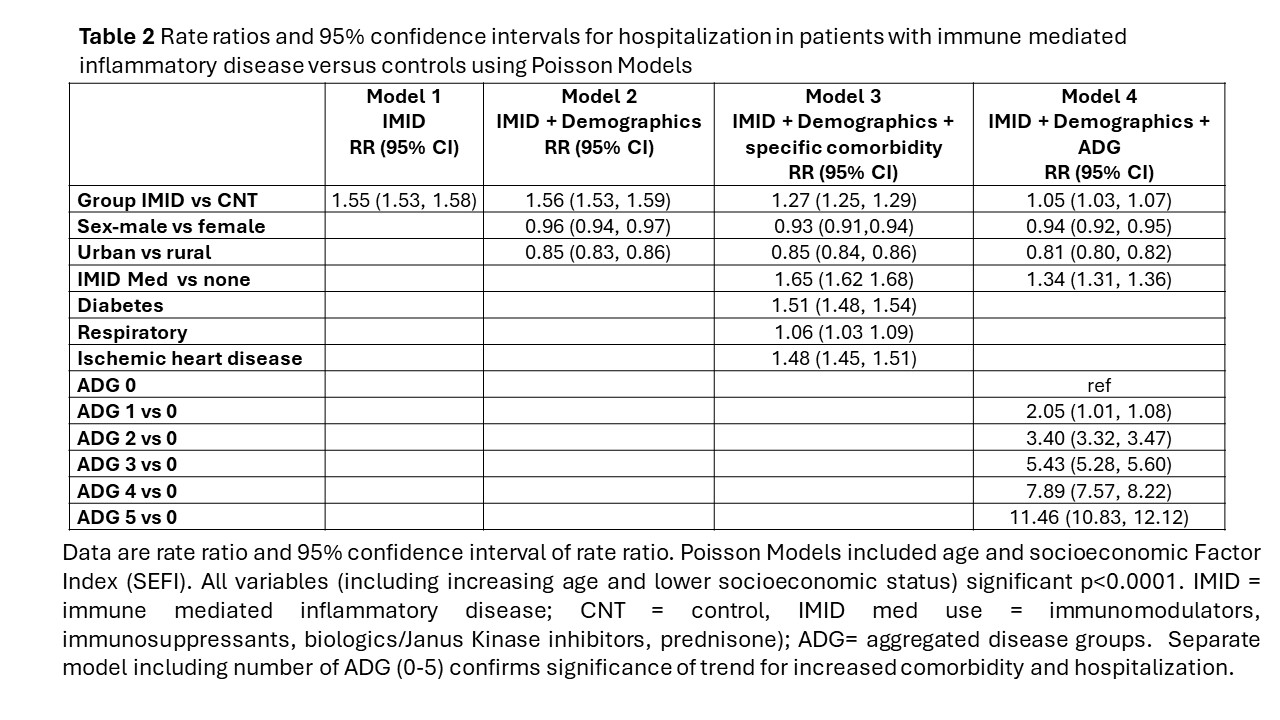
Methods: Using a cohort study design, administrative health records were used to identify people with IMID (n=48698; RA= rheumatoid arthritis n=10405, SARDS= systemic autoimmune rheumatic disease n=5888, IBD = inflammatory bowel disease n=7911, MS= multiple sclerosis n=3665, PsO= psoriasis n=23948) who were matched (1:5) by age, sex and region to general population controls without these IMIDs (CNTs n=243490). Between Jan 1st, 2000, and March 31st 2022, rates of COVID-19 vaccine administration were compared between IMIDs and CNTs. Logistic regression models compared vaccine uptake (≥1 dose) between IMIDs and CNTs. Odds ratios (OR) and 95% confidence intervals (CI) reported. Poisson regression models compared COVID-19 hospitalizations in this period between IMIDs and CNTs. Rate ratios and 95% CI reported. Models were adjusted for age, sex, region, socioeconomic factor index (SEFI), immunomodulatory drugs, and comorbidity. Separate models assessed the impact of comorbidities using John Hopkins Aggregated Diagnosis Groups (ADGs) or specific comorbidities (diabetes, respiratory disease, ischemic heart disease).
Results: We identified 48698 people with an IMID [mean (standard deviation -sd) age 55.65 (16.8) years, 61.2% female. Most (64%) resided in urban centers and had favorable SEFI scores (mean (sd) -0.13 (0.89)]. Most received a least one COVID-19 vaccine (IMID 87.67% vs CNT 84.70% p< 0.001). IMIDs had more vaccines than controls [IMID vs CNTs single vaccine 374 (0.77%) vs 1783 (0.73%), 2 vaccines 8523 (17.5%) vs 47766 (19.62%), 3 vaccines 33795 (69.4%) vs 156683 (64.35%); p< 0.0001]. Age, female sex, higher socioeconomic status, urban residence, IMID medication, and comorbidities were associated with increased vaccine uptake (Table 1). IMID patients had more hospitalizations for COVID-19 than controls [IMID 79 (77.8-80.2)/100000 vs CNTs 51 (50.5-51.3) /100000 (rate ratio 1.55; 95% CI 1.53, 1.58)]. In adjusted models age, SEFI, IMID medications, and comorbidity were associated with COVID-19 hospitalization risk (Table 2). Increasing comorbidity (increased ADGs) further increased hospitalization. Only 3/721 hospitalizations occurred and all within 7 weeks of COVID19 vaccination.
Conclusion: Compared to the general population, people with diagnosed IMID had greater COVID-19 vaccine uptake. Hospitalization rates were driven mainly by age, worse socioeconomic status, and immunomodulating treatment. Persons with IMID were at greater risk for hospitalization despite higher vaccine uptake. Given that SARS-CoV-2 is now chronically endemic, these new data may be important for guiding vaccination recommendations.
To cite this abstract in AMA style:
Hitchon C, Taylor C, Bernstein C, Peschken C, Avina-Zubieta J, Bernatsky S, Kaplan G, Lacaille D, Widdifeild J, Marrie R. COVID-19 Vaccination and Hospitalization Rates Differ Between People with Diagnosed Immune Mediated Inflammatory Disease and the General Population: A Population-based Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/covid-19-vaccination-and-hospitalization-rates-differ-between-people-with-diagnosed-immune-mediated-inflammatory-disease-and-the-general-population-a-population-based-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-vaccination-and-hospitalization-rates-differ-between-people-with-diagnosed-immune-mediated-inflammatory-disease-and-the-general-population-a-population-based-study/