Session Information
Date: Tuesday, November 9, 2021
Title: Pediatric Rheumatology – Clinical Poster III: Miscellaneous Rheumatic Disease (1614–1644)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Infection with novel coronavirus (COVID-19) in children, unlike adults, is generally asymptomatic or causes mild disease although some may develop severe illness. In particular, pediatric rheumatology patients may be at higher risk due to their immunosuppression. There are few publications describing COVID-19 infection among children with rheumatologic diseases. The Southwest region has had multiple COVID-19 surges and less prominent mitigation than other parts of the country with perhaps greater risks to children with chronic illness. This study reports on COVID-19 infections, risk factors for morbidities, and outcomes in pediatric rheumatology patients cared for in a large urban tertiary pediatric health system.
Methods: With approval from the Institutional Review Board of Baylor College of Medicine, a retrospective review was conducted of pediatric rheumatology patients followed at Texas Children’s Hospital (TCH) from March 10, 2020 to April 10, 2021. We abstracted charts for demographic data, rheumatologic diagnoses, immunomodulatory therapies, COVID-19 infection and hospital course if admitted. The SlicerDicer Epic tool (Madison, WI) was used to assess number of active patients seen during the study period. Analyses were performed with Stata v16.1. Categorical variables were compared using Fisher’s Exact test.
Results: There were approximately 1593 pediatric rheumatology patients actively followed during the study, including 800 JIA patients and 204 lupus patients. During the study period, 43 had COVID-19 infection (43/1593, 2.7%), with an incidence of 2.1% in JIA patients and 5.9% in lupus patients. Table 1 summarizes demographic and clinical characteristics. Twenty-one held their rheumatologic therapy; of these, 5 patients (24%) had a flare of their condition. No patient developed MIS-C.
Eight patients were hospitalized, 3 (37.5%) whom required intensive care. The median length of stay was 6.5 days (1-81), and 8 days (2-42) for ICU patients. Majority were Hispanic (75%), and 6 (75%) were female. There was a statistically significant association between obesity with hospitalization as well as Steroid dose of ≥10 mg; all 3 ICU patients were taking ≥10 mg. No association was found between specific DMARD or biologic and hospitalization.
The characteristics and course of 3 ICU patients, 2 with SLE and 1 with a rare autoinflammatory syndrome, are presented in Table 2. All presented with fever ≥101°F (≥38.3°C), and 2 required supplemental O2. One lupus patient required mechanical ventilation and passed away from respiratory failure.
Conclusion: In a county with a high COVID-19 prevalence, only a small percentage of pediatric rheumatology patients presented to medical care with confirmed infections. Most had mild courses that did not affect their underlying disease. As per adult experiences, obesity and higher steroid doses were observed in admitted patients. Children with SLE and from underrepresented minorities represented a large proportion of those affected, suggesting a significant role of socioeconomic factors with increased risk of exposures. The effect of vaccine protection on pediatric rheumatology patients will be studied during the upcoming year.
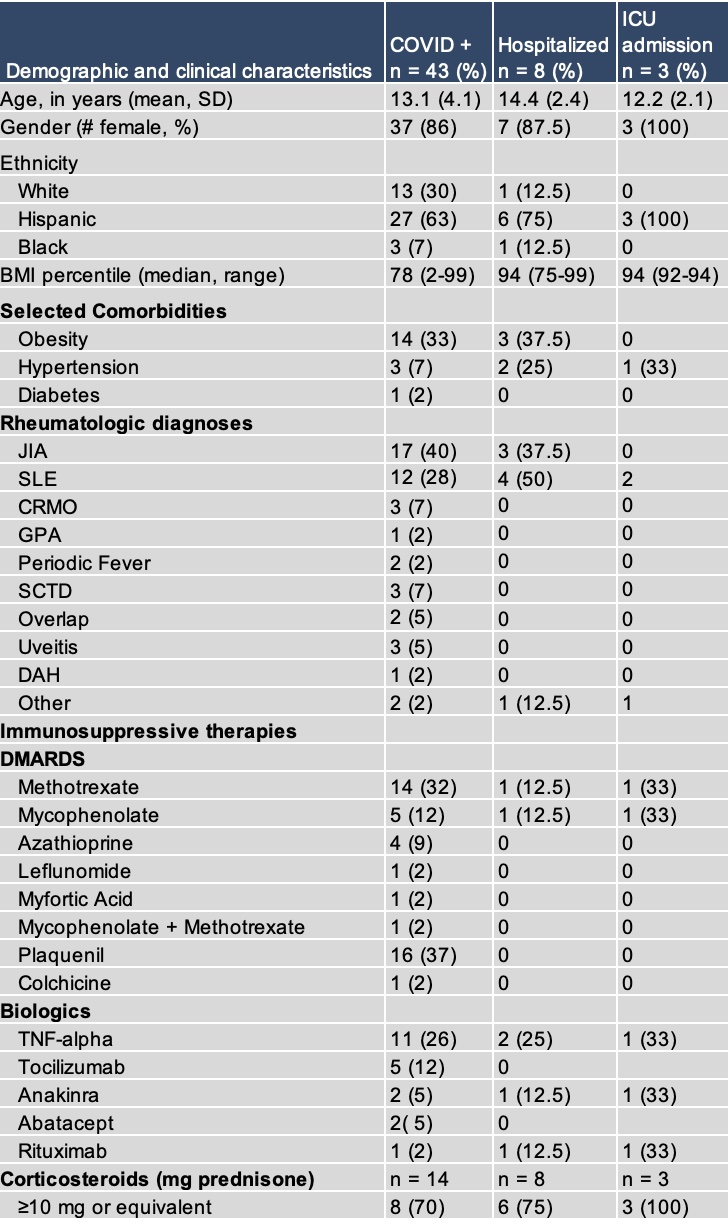 Table 1. Demographic and clinical characteristics of COVID + pediatric rheumatology patients.
Table 1. Demographic and clinical characteristics of COVID + pediatric rheumatology patients.
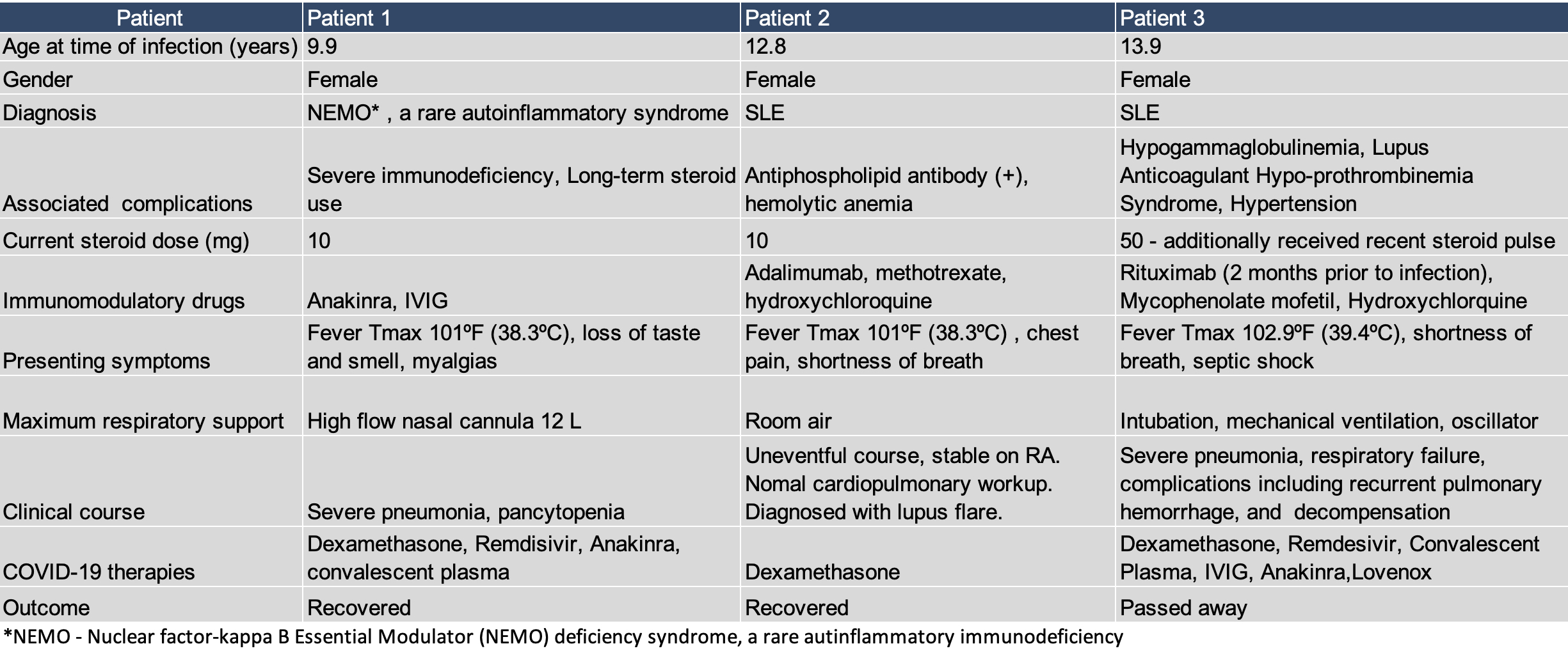 Table 2. Characteristics and clinical course of 3 patients admitted to the ICU for COVID_19
Table 2. Characteristics and clinical course of 3 patients admitted to the ICU for COVID_19
To cite this abstract in AMA style:
Kok E, Curry M, Ramirez A, Muscal E, DeGuzman M. Covid-19 Infection Among Pediatric Rheumatology Patients: A Single Center Experience [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/covid-19-infection-among-pediatric-rheumatology-patients-a-single-center-experience/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-infection-among-pediatric-rheumatology-patients-a-single-center-experience/
