Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Initial studies of SLE patients with COVID-19 revealed an increased risk for severe disease in people with distinct demographic features such as advanced age and/or underlying comorbidities comparable to that of the general population. However, uncertainty remains around the real impact SARS-CoV-2 has in SLE. In this context, we conducted a cross-sectional survey in SLE patients who follow at our tertiary care lupus cohort.
Methods: We designed a questionnaire using the REDCap tool to capture information about demographics, clinical and serological variables related to SLE and COVID-19. The survey was sent between June 1st to August 31st, 2020 to 87 participants. Additional information was gathered from the lupus registry database. After the survey ended subjects underwent SARS-CoV-2 IgG antibody testing.
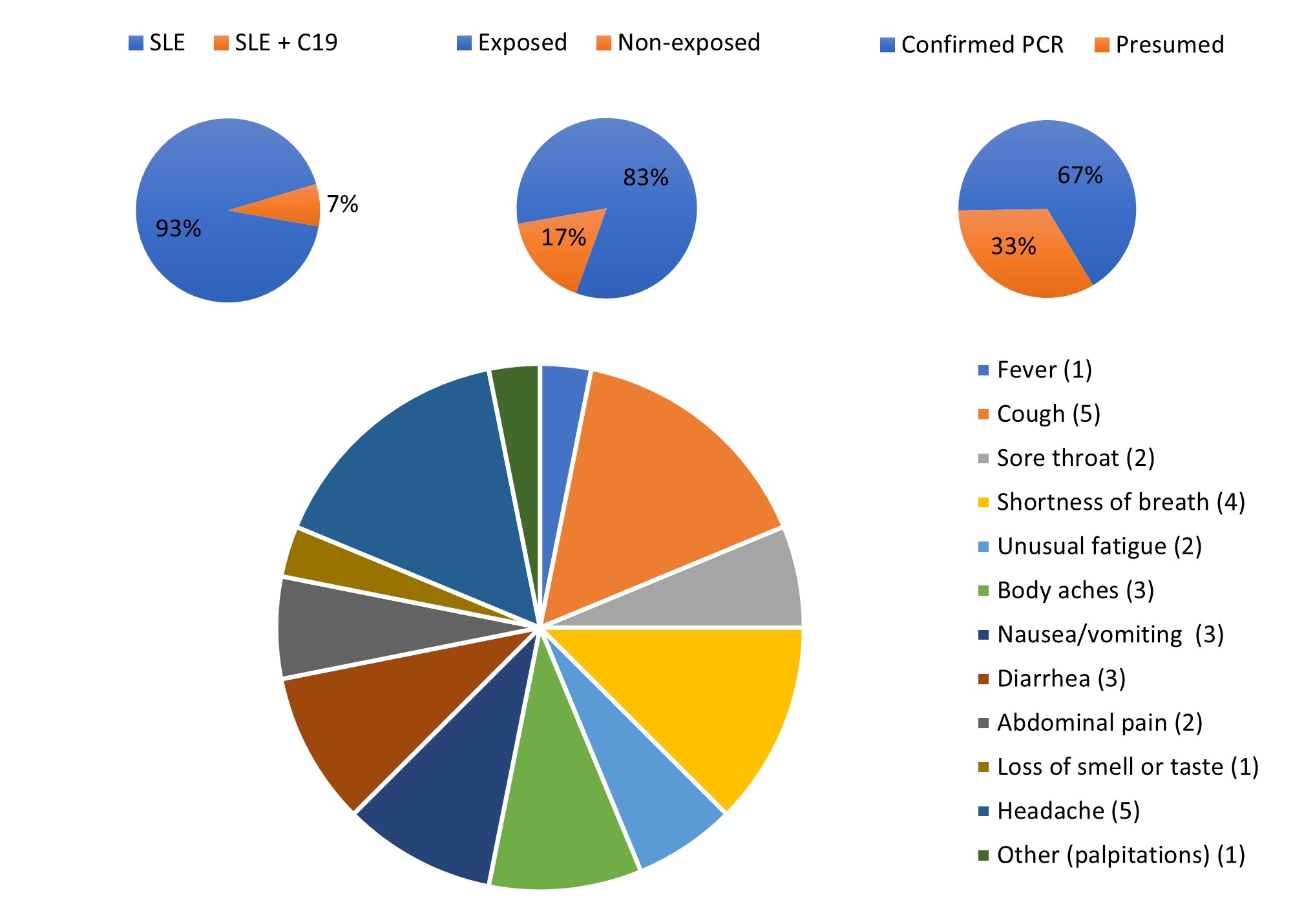
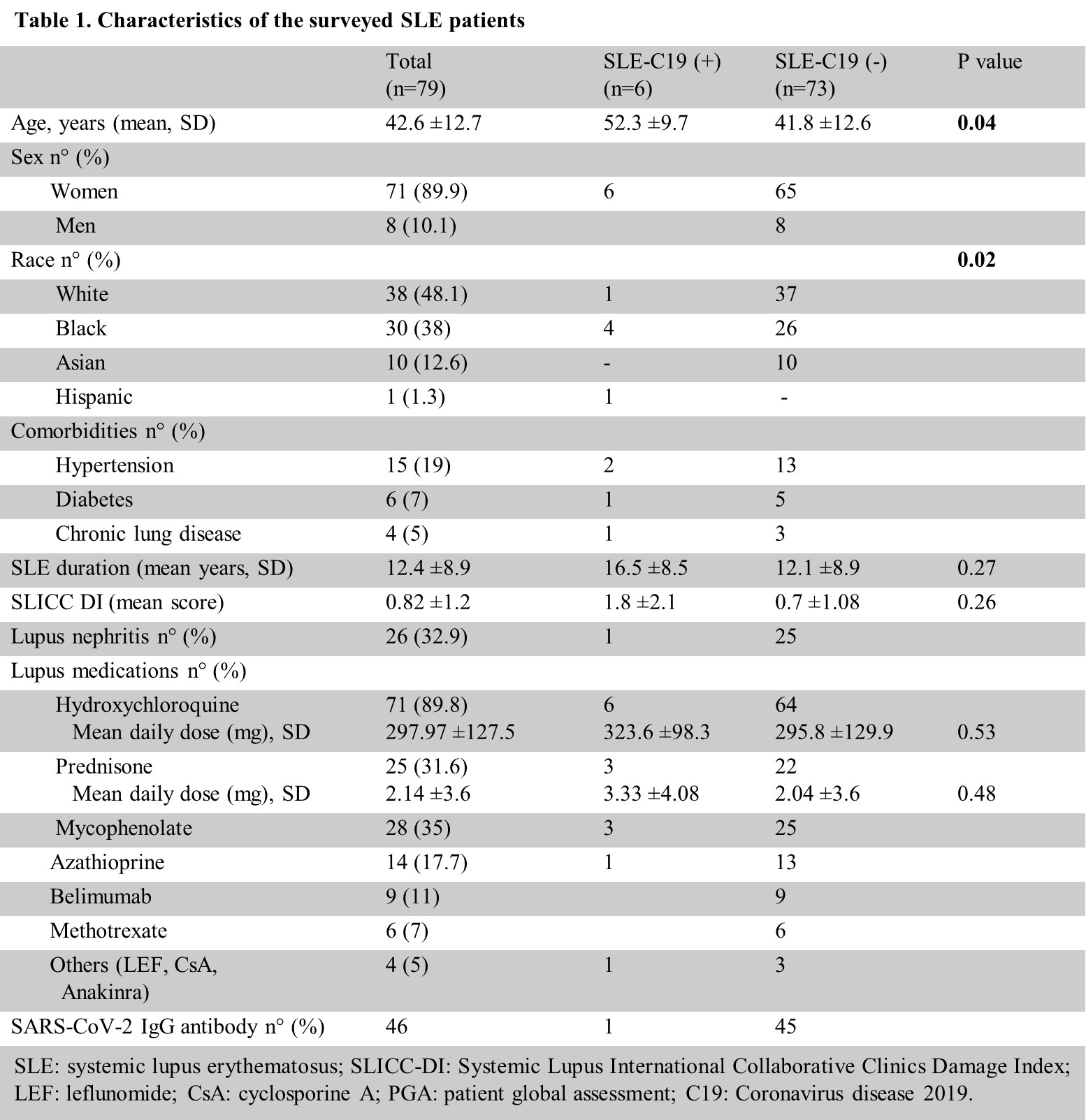
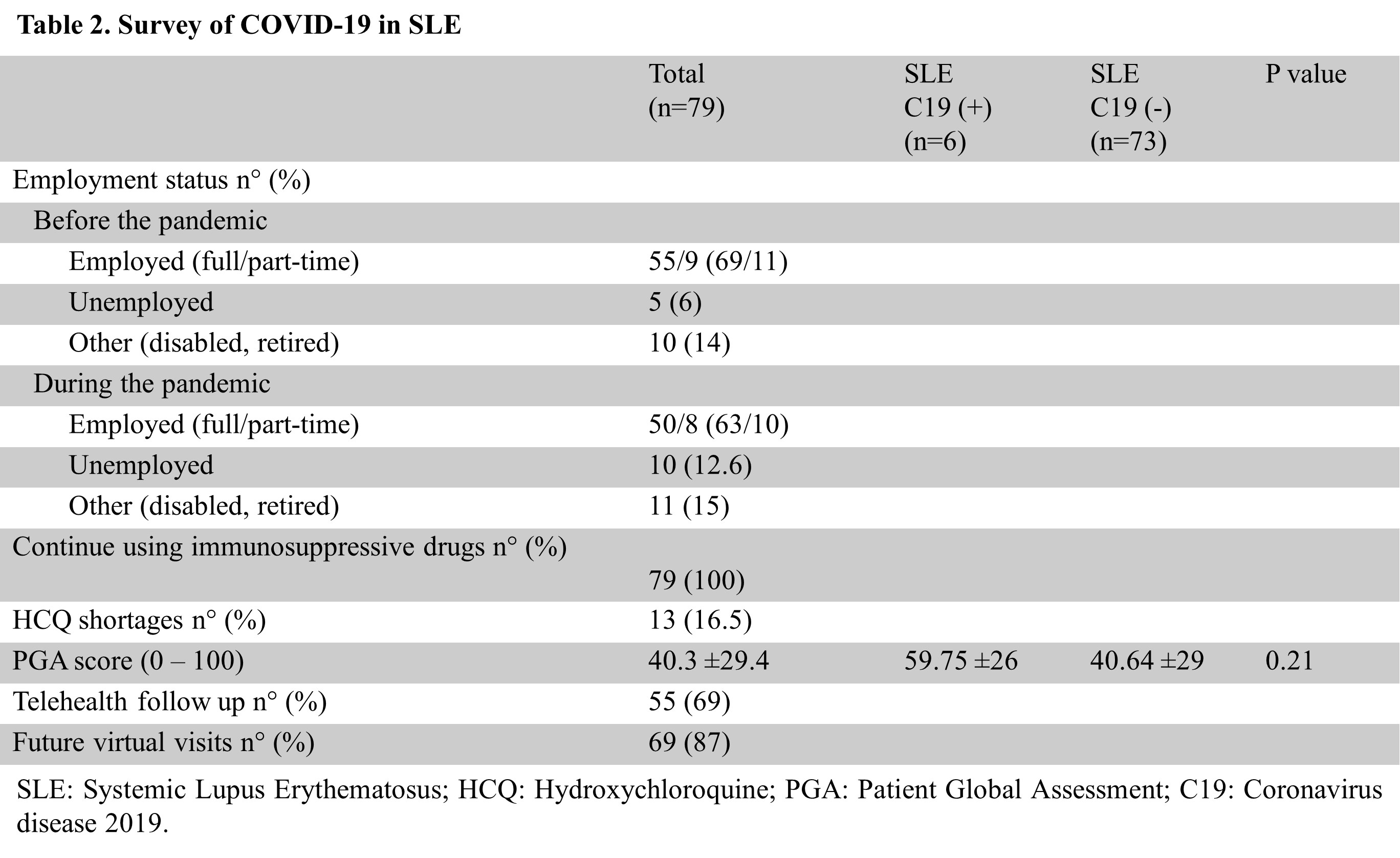
Results: A total of 79 subjects completed the survey. From these, 6 patients developed COVID-19 infection with many of them disclosing an epidemiologic link. All infected patients were female and the mean age was significantly higher in COVID-19 patients compared to those who did not get infected (p 0.04). We also found a significant relationship between COVID-19 status and race (p 0.02) with the majority of the infected individuals having black ancestry. COVID-19 serology was tested in 46 individuals, showing only one positive result in someone who reported COVID-19 infection. Interestingly, among 4 infected subjects whose serology was obtained only one had evidence of persistent immunity against SARS-CoV-2 10 months after the infection. Additionally, we observed a numeric trend in patients’ global disease activity (60 v 41), SLE duration (17 v 12 years), SLICC-DI score (1.8 v 0.7), and mean daily dose of prednisone (3 v 2 mg) in COVID-19 patients compare to non-infected subjects, respectively. In regards to COVID-19 features in SLE, the most common symptoms were headache, shortness of breath, and cough. Despite a prolonged illness and a relative more severe SLE, the majority of infected patients presented with a favorable disease course including the patient who was hospitalized. Moreover, the use of immunosuppressive drugs was not found to be associated with severe infection. COVID-19 related hydroxychloroquine shortage affected up to 16.5% of SLE patients, but at least short-term consequences were not evident. Lastly, we identified that 69% of the respondents were able to continue medical care through telehealth during the surge, and 87% were eager to make use of telemedicine services in the foreseeable future.
Conclusion: Despite study limitations, our data confirm that age and race are important risk factors for COVID-19 infection in SLE. Importantly, we also noted that neither underlying SLE nor the use of immunosuppressive drugs was found to be risk factors for severe COVID-19 illness though further studies are needed. Finally, our results demonstrated that having COVID-19 infection does not necessarily mean prolonged immunity as this can wane over time. In any case, as the pandemic continues to unfold, rheumatologists should continue stressing preventive measures, recommending vaccination, and offering optimal virtual care when needed to avoid undesirable outcomes.
The prevalence of COVID_19 in patients with SLE (SLE, SLE+C19) is shown on the upper leftmost panel. Exposure history and PCR positivity in SLE patients with COVID_19 are plotted in the middle and rightmost panel, respectively. The prevalence of different symptoms in patients with SLE and COVID_19 are depicted in the lower panel.
To cite this abstract in AMA style:
Rubio J, krishfield S, Kyttaris V. COVID-19 Impact Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/covid-19-impact-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-impact-among-patients-with-systemic-lupus-erythematosus/