Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cost-related medication non-adherence (CRN), a measure of drug affordability, refers to a patient’s inability to adhere to a prescribed medication regimen due to high medication costs or lack of insurance coverage. Financial burden may lead patients to skip doses, reduce dosages, or delay refilling their prescriptions, which can have negative effects on their health outcomes. In this study, we aimed to investigate CRN in a nationally representative sample of US adults with chronic arthritis.
Methods: We utilized data from the National Health Interview Survey (NHIS) spanning the years 2013 to 2018. By applying survey weights, we calculated the proportion of individuals experiencing CRN among those with and without chronic arthritis of any type. We also calculated the proportion of CRN among individuals with cancer (any type), diabetes mellitus (any type), and heart disease (any type) as comparison groups. Additionally, we calculated the proportion of CRN in subgroups based on gender and race/ethnicity. To ensure accurate calculations, we limited the denominator samples to individuals who received at least one prescription drug. Significant differences were determined using 95% confidence intervals. Data analyses were performed using Stata and Python.
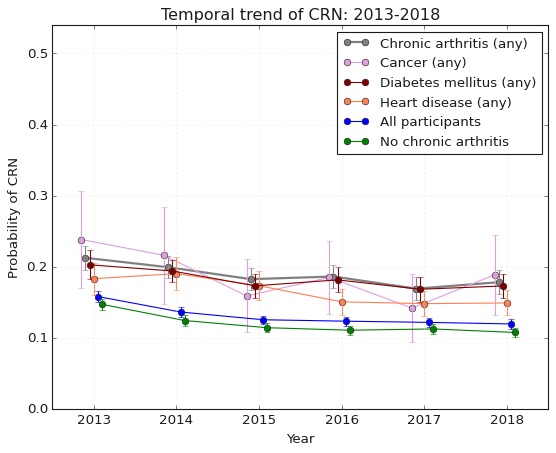
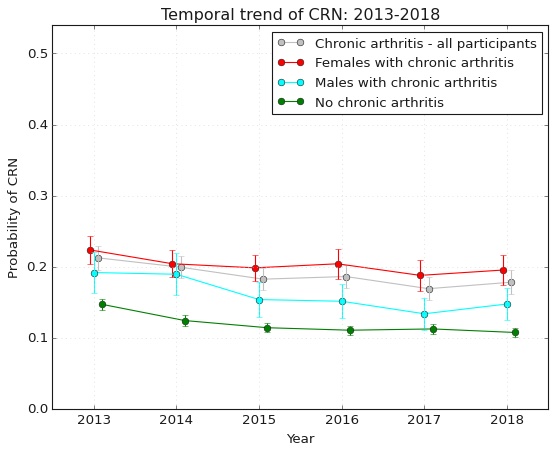
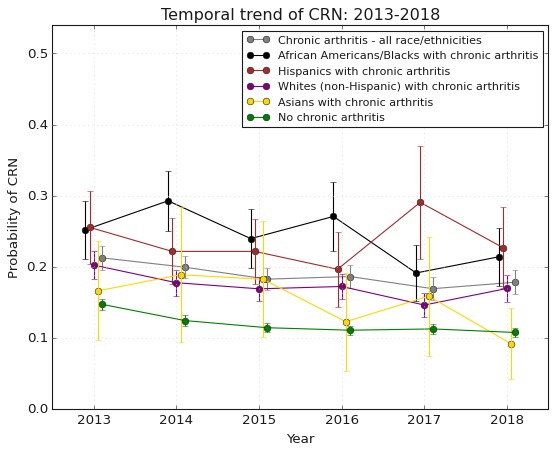
Results: The study included 163,579 participants without chronic arthritis and 26,534 participants with chronic arthritis, of which 17,840 were females with chronic arthritis. Among those with chronic arthritis, there were 19,047 non-Hispanic Whites, 3,917 African Americans/Blacks, 2,497 Hispanics, 625 Asians, and 421 individuals belonging to other races/ethnicities. From 2013 to 2018, the likelihood of experiencing CRN showed a downward trend among individuals with chronic arthritis (21.26% vs. 17.83%, p< 0.05) as well as those without chronic arthritis (14.72% vs. 10.76%, p< 0.05). CRN was consistently higher across all years in individuals with chronic arthritis versus those without, and the likelihood of experiencing CRN in this group was comparable to that of individuals with cancer and diabetes (Figure 1). Throughout 2013 to 2018, females with chronic arthritis were significantly more likely to experience CRN than males, and the gender disparities in CRN widened during this period (Figure 2). Furthermore, African Americans/Blacks and Hispanics exhibited trends indicating a higher likelihood of experiencing CRN compared to non-Hispanic Whites and Asians. Nonetheless, those differences were not statistically significant throughout all the years analyzed. (Figure 3).
Conclusion: The likelihood of experiencing CRN is gradually decreasing among individuals with and without chronic arthritis. However, individuals with chronic arthritis have a similar likelihood of experiencing CRN compared to those with cancer and diabetes mellitus. Furthermore, our findings raise concerns about potential gender and racial/ethnic disparities in the risk of CRN among US adults with chronic arthritis. In light of these findings, it is crucial to conduct further research and implement targeted policy solutions to address such disparities, ensuring equitable access to affordable medications for all individuals with chronic arthritis.
To cite this abstract in AMA style:
Ara A, Chenoweth M, Scannell C, FitzGerald J. Cost-Related Medication Non-Adherence Among US Adults with Chronic Arthritis: Trends, Comparisons, and Disparities [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/cost-related-medication-non-adherence-among-us-adults-with-chronic-arthritis-trends-comparisons-and-disparities/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-related-medication-non-adherence-among-us-adults-with-chronic-arthritis-trends-comparisons-and-disparities/