Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Juvenile Idiopathic Arthritis (JIA) is the most common rheumatologic disease of childhood. Active joint count (AJC) is one of the key JIA Core Set variables. However, AJC is a subjective measurement with poor-to-moderate inter-rater agreement. Musculoskeletal Ultrasound (MSUS) is a radiation-free, objective imaging tool currently being used to assess joint inflammation. A novel joint-specific MSUS scoring system for JIA was recently proposed[1]. The aims of this study are: 1. Determine the frequency of subclinical synovitis as per MSUS in all peripheral joints in JIA, 2. Correlate AJC as determined by expert clinician physical examination with moderate to severe MSUS synovitis, 3. Examine the correlation between MSUS synovitis and Juvenile Arthritis Disease Activity Score (JADAS) and patient-reported outcomes
Methods: Data obtained from a previously described study looking to determine the key joints to perform a MSUS examination in JIA[1] was used for the current analysis. Briefly, JIA patients presenting with an AJC >4 and able to perform MSUS within 1 week of starting a Disease-modifying Antirheumatic Drug were eligible for this study. Clinical data including physician global assessment (PhGA), patient global assessment (PGA), patient pain visual analogue scale (VAS) and the Child Health Assessment Questionnaire (CHAQ) were obtained. A comprehensive AJC examination and a 42 joint MSUS examination by an American College of Rheumatology MSUS certified pediatric rheumatologist were performed at baseline and at 3 months. Gray-scale B mode and Power Doppler (PD) images were obtained for each view. Images were scored following a semiquantitative scoring system ranging from 0-normal to 3-severe. Subclinical synovitis was defined as grade 2 and 3 synovitis appreciated by MSUS only. Clinical-JADAS 10 (cJADAS-10) was calculated by the addition of PhGA, PGA, and AJC up to 10 joints. Pearson correlation was used to assess the correlation between AJC and subclinical synovitis. Spearman’s correlation coefficients were calculated to determine the association between MSUS synovitis, cJADAS-10 and patient-reported outcomes
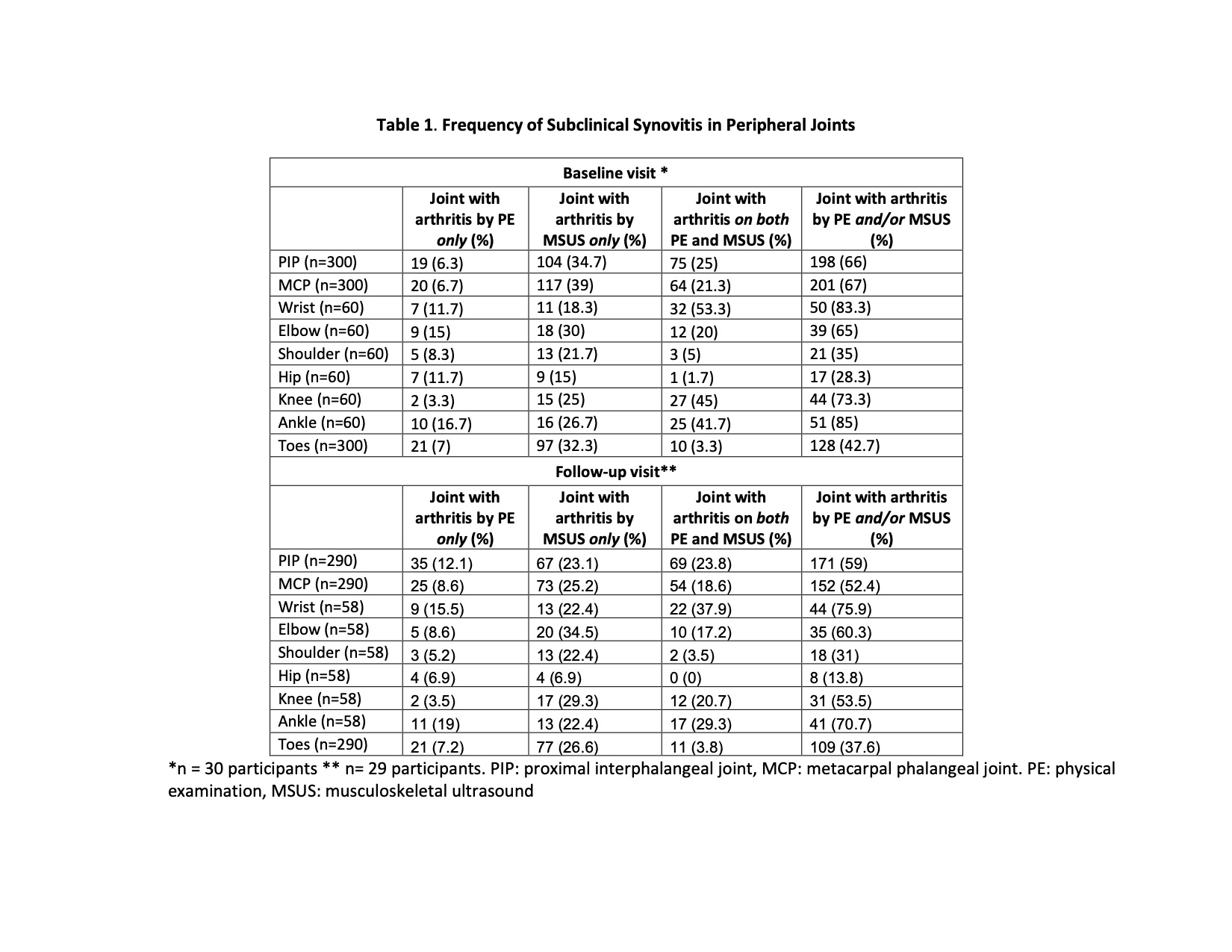
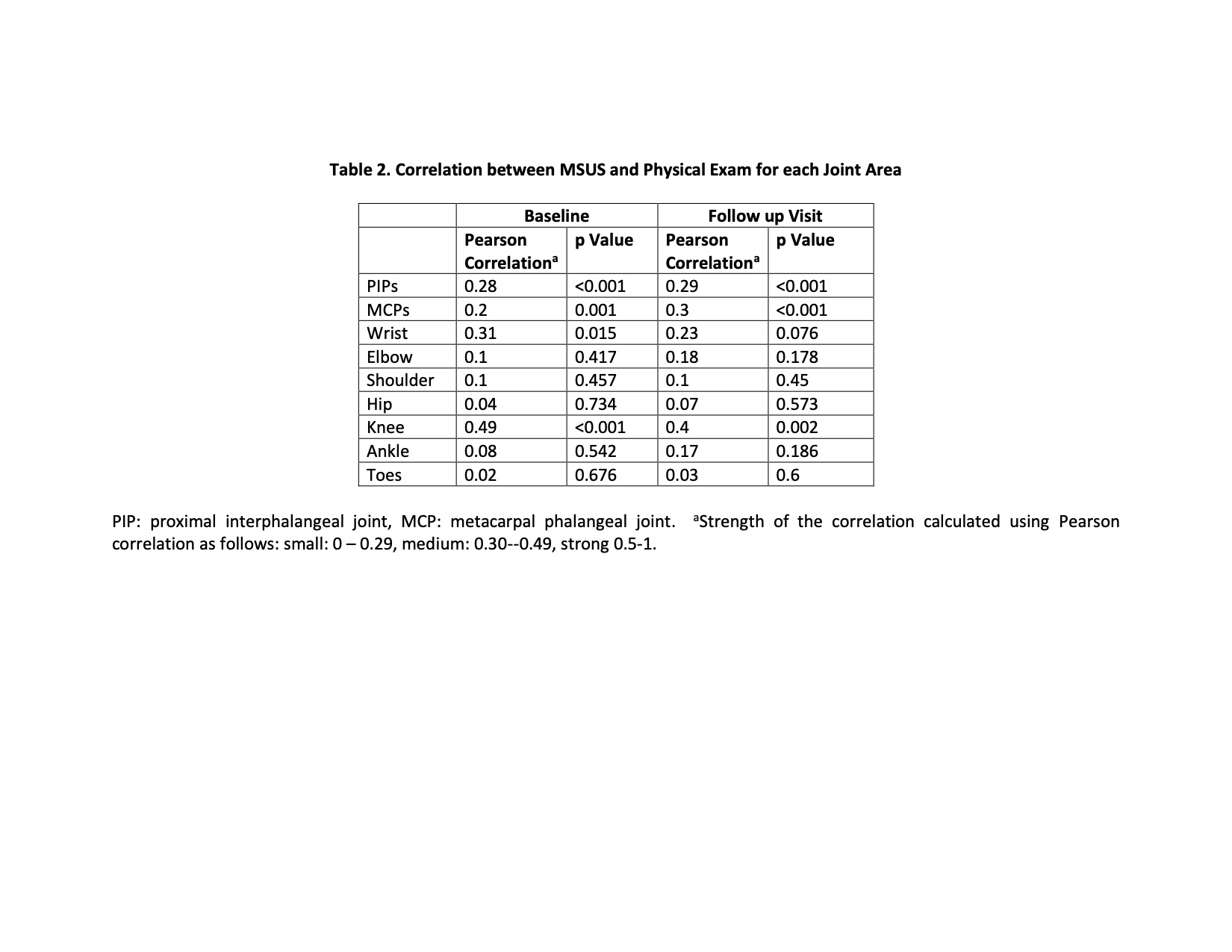
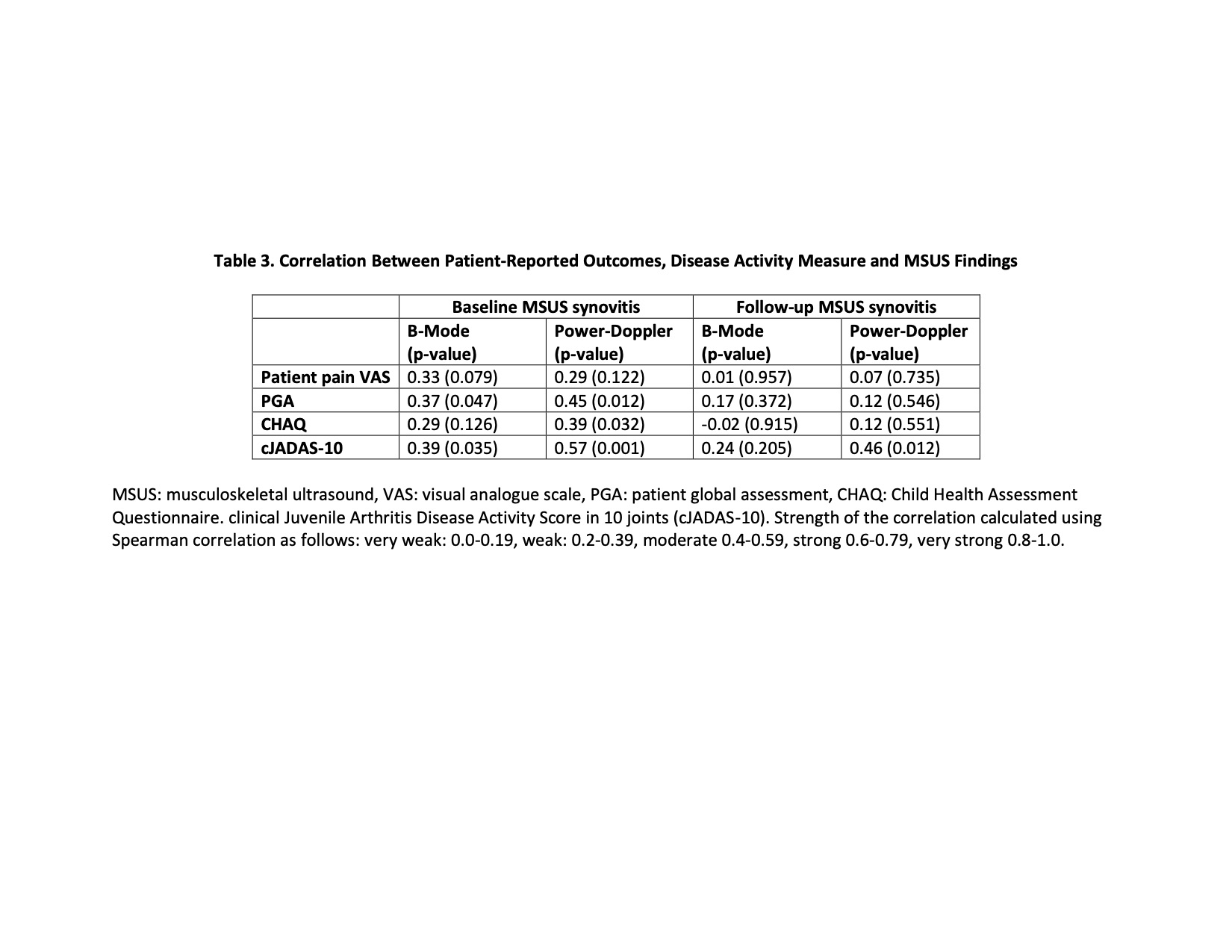
Results: A total of 30 patients were enrolled. Table 1 shows the frequency of subclinical synovitis per joint. In general, MSUS detects moderate to severe synovitis in about 25% of the joints determined as normal by physical exam. Except for the knee where the correlation between MSUS synovitis and AJC was moderate, the correlation between MSUS and AJC for all other peripheral joints was slight to fair (Table 2). MSUS synovitis and patient reported outcomes including CHAQ, patient pain VAS and PGA had slight to fair correlation for B-Mode and moderate correlation for PD. Correlation between MSUS and cJADAS-10 was moderate for both B Mode and PD images. (Table 3)
Conclusion: Subclinical synovitis is commonly observed in a cohort of newly diagnosed JIA patients with greatest differences in digits. The fair to moderate correlation of MSUS synovitis with cJADAS-10 and patient-reported outcomes, suggest that MSUS assesses a different, possibly more objective, domain not determined by traditional JIA outcome measurements. MSUS has the potential to support the diagnosis and assessment of JIA
To cite this abstract in AMA style:
Vega-Fernandez P, Oberle E, Henrickson M, Huggins J, Altaye M, Cassedy A, Roth J, Ting T. Correlation of Subclinical Synovitis with Juvenile Idiopathic Arthritis Outcome Measurements [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/correlation-of-subclinical-synovitis-with-juvenile-idiopathic-arthritis-outcome-measurements/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/correlation-of-subclinical-synovitis-with-juvenile-idiopathic-arthritis-outcome-measurements/