Session Information
Date: Sunday, November 7, 2021
Title: Measures & Measurement of Healthcare Quality Poster (0623–0659)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: In a prior survey of providers and patients (Chakravarty 2014), it became apparent that clear gaps exist in provider-patient communication, affecting the delivery and success of contraceptive counseling for rheumatology patients. It is unclear how best to examine the prevalence of contraceptive counseling in clinical practice, but previous work has mainly relied on either medical chart review or patient survey to determine if counseling occurred. In this study we directly compare provider documentation of counseling with patient reported experience to assess if patient perspectives align with provider documentation. To our knowledge, this is the first study to investigate the prevalence of counseling in this manner.
Methods: Females of childbearing potential (ie, 18-50 years; no self-reported history of surgical sterilization, hysterectomy, menopause) with an established autoimmune condition were invited to complete on-line questionnaires. All patients were asked if they had ever received contraception counseling or been counseled about the potential pregnancy risks of their medications. In addition, a review of electronic medical records was performed for all patients to identify provider documentation of contraceptive counseling. An anonymous on-line questionnaire was also given to clinical providers (8 rheumatology attending physicians, 6 rheumatology fellows and 2 rheumatology nurse practitioners) to assess their perception of how often they provide contraception counseling. Agreement between patient reported counseling and provider documentation of counseling was analyzed by Cohen’s kappa (where k=1 is perfect agreement and k=0 is no agreement).
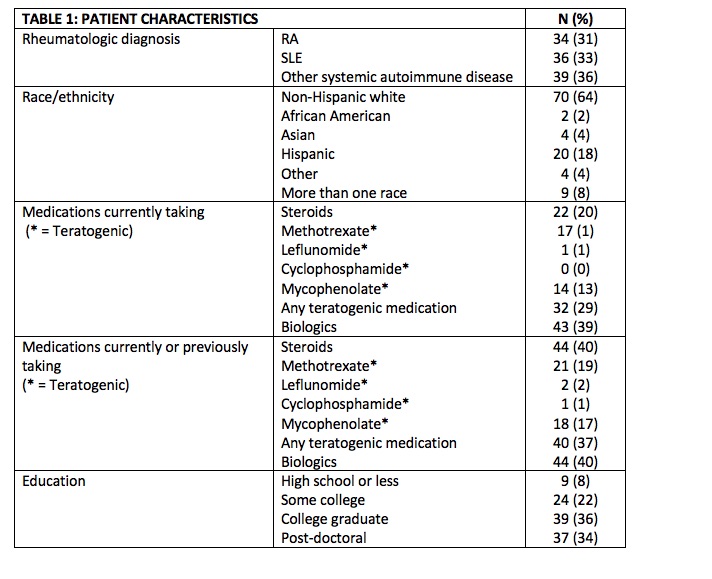
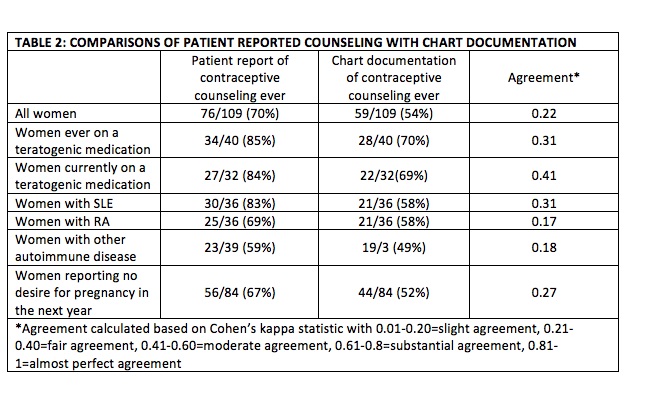
Results: We surveyed 109 women. The mean age was 34 years, 29% were currently or previously taking a teratogenic medication, 64% were non-Hispanic white and 92% had higher than a high school education. Overall, agreement was poor between women reporting having received contraception counseling and women with chart documentation of contraception counseling (Table 2, 70% vs. 54%, k=0.22). Agreement was slightly higher for women taking teratogenic medications (85% vs. 70%, k=0.41) and for women with lupus (83% vs. 58% k=0.31). Providers identified patient complexity as the major barrier to speaking to patients about family planning.
Conclusion: Women in an academic rheumatology practice were more likely to report having received counseling on contraception than was documented in their medical chart, suggesting that chart documentation of counseling may underestimate the true prevalence of this type of counseling that occurs in clinical care. More robust correlation was seen in patients with SLE or those currently on a teratogenic medication indicating that documentation may be more likely to occur for patients at risk for poor outcomes in the event of an unplanned pregnancy. These data showcase the need to improve the ease of documentation of contraception counseling in the medical record and continued commitment to the provision of discussions surrounding contraception with our patients.
To cite this abstract in AMA style:
Carvajal Bedoya G, Skorupa T, Sturm K, Kwag J, Demoruelle K, Zell J. Correlation Between Provider Documentation and Patient Experience with Contraceptive Counseling in an Academic Rheumatology Practice [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/correlation-between-provider-documentation-and-patient-experience-with-contraceptive-counseling-in-an-academic-rheumatology-practice/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/correlation-between-provider-documentation-and-patient-experience-with-contraceptive-counseling-in-an-academic-rheumatology-practice/