Session Information
Date: Wednesday, November 16, 2016
Title: Health Services Research II
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose : We have recently found that myocardial infarction (MI) risk was similar among age- and sex-matched SLE patients compared to diabetes mellitus (DM) patients within a U.S. Medicaid cohort. However, little is known about rates and relative risks of coronary revascularization (CR) procedures, such as coronary artery bypass grafting (CABG) and percutaneous coronary interventions (PCI), among SLE compared to DM patients. We compared rates and relative risks of CR procedures among patients with SLE and DM enrolled in Medicaid.
Methods : We utilized Medicaid Analytic eXtract (MAX) data, containing billing claims for Medicaid patients from 29 most populated U.S. states from 2007-2010. We identified adults aged ≥18-65 years with prevalent SLE or DM (≥3 ICD-9 codes for SLE or DM, each separated by ≥30 days) and >6 months enrollment prior to 3rd code (=index date). We performed 1:2 matching (SLE:DM) by age (month/year), sex, and index date. Sociodemographic data and medical and cardiac comorbidities were collected during the baseline period (6 months prior to and including index date). Outcomes were assessed after index date, including CABG, PCI, and combined CABG or PCI. Subjects were followed to first procedure, death, Medicaid disenrollment, or end of follow-up. We used Cox sub-distribution regression models to calculate hazard ratios (HRSD) of undergoing CR procedures, accounting for the competing risk of death and adjusting for sociodemographics and cardiac and medical comorbidities.
Results : 32,089 prevalent SLE patients were matched to 64,178 prevalent DM patients. In both cohorts, 92.8% were female and mean age was 41.3 (±12.1) years. There were more Blacks (41.1 vs. 30.5%) and fewer Whites (36.3 vs 45.1%) in the SLE vs. DM cohort. Mean follow-up was 1.67 (±1.03) years for SLE and 1.79 (±1.07) years for DM. Cardiac risk factors at baseline were more prevalent among DM vs. SLE patients: hypertension (38.0 vs. 33.7%), hyperlipidemia (22.5 vs. 10.6%), and obesity (11 vs. 4.5%). PCI rates were nearly 10-fold those of CABG rates in each cohort (Table). Annual rates of CABG and PCI were much higher among SLE than DM patients. Age- and sex-adjusted risks of CR procedures, particularly CABG, were higher among SLE than DM patients. Multivariable adjustment attenuated relative risks slightly. The multivariable-adjusted HRSD for CABG was 1.83 (95%CI 1.48-2.25) and for PCI was 1.23 (95%CI 1.15-1.31) in SLE vs. matched DM patients.
Conclusion : Despite similar MI risks among SLE and DM patients, SLE patients had substantially higher rates of PCI and CABG compared to age- and sex-matched DM patients. SLE patients had > 80% increased risk of CABG compared to DM patients. While the etiology of these differences is not clear, they suggest that underlying cardiovascular disease may more severe or more likely to come to medical attention among SLE than similar age and sex DM patients. 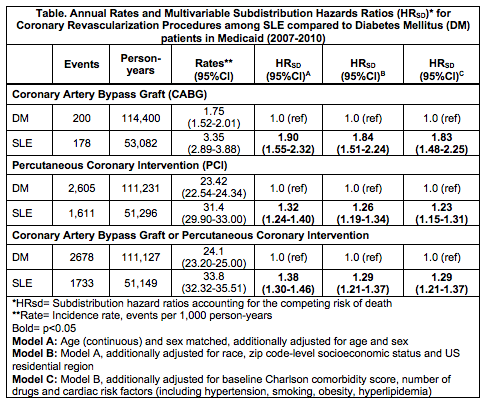
To cite this abstract in AMA style:
Barbhaiya M, Feldman CH, Chen SK, Guan H, Lin TC, Fischer MA, Solomon DH, Everett BM, Costenbader KH. Coronary Revascularization Procedure Rates and Risks Among Patients with Systemic Lupus Erythematosus Compared to Those with Diabetes Mellitus in a Nationwide Medicaid Cohort [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/coronary-revascularization-procedure-rates-and-risks-among-patients-with-systemic-lupus-erythematosus-compared-to-those-with-diabetes-mellitus-in-a-nationwide-medicaid-cohort/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/coronary-revascularization-procedure-rates-and-risks-among-patients-with-systemic-lupus-erythematosus-compared-to-those-with-diabetes-mellitus-in-a-nationwide-medicaid-cohort/
