Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: An important proportion of patients with Idiopathic inflammatory myopathies (IIM) are at risk of developing refractory disease, which predispose them to cumulate damage, treatment toxicity and disability. Therefore, there is a crucial need for the early identification of patients at risk of refractory disease, which is the aim of this study.
Methods: For this prospective cohort study, we recruited 200 patients who fulfilled the ACR/EULAR classification criteria for IIM in the Myositis Translational Research Cohort Salvador Zubirán (MYOTReCSZ) from 2015 to 2024. We excluded patients with juvenile dermatomyositis and inclusion body myositis. Patients were prospectively followed-up to assess the disease activity, damage accrual, and changes in immunosuppressive therapy. At baseline, which was the time of recruitment in the cohort, we assessed the myositis specific and associated antibodies using the Lineblot from Euroimmune. The primary outcome was the development of refractory disease, defined as failure to induce remission after a course of treatment with glucocorticoids at optimal doses or lack of improvement after using a second-line therapy. We evaluated the baseline predictors of refractory disease with the multivariate logistic regression model showing the lowest Akaike Information Criterion and calculated the Odds Ratios (OR) with 95% confidence intervals (95% CI). We estimated the cut-off points for each of these variables and created the ReMPI (Refractory Myositis Predictive Index), assigning a numerical value to each OR. We calculated the ideal cutoff point of the ReMPI, its optimism-corrected predictive capacity and performed an internal validation using bootstrapping.
Results: Most patients were women (73.5%). The median and interquartile range (IQR) of age at recruitment was 44.5 years (32.0-55.5) and the most frequent diagnosis was dermatomyositis (84%). Sixty-four patients (32%) had refractory disease. At baseline, patients with refractory disease had more frequently anti-TIF1-g antibodies (11 [17.1%] vs 5 [3.6%], P=0.001), and a shorter time from disease onset to diagnosis (4 months [1.0-8.2] vs 6 [2.0-10.5], P=0.05). Also, they had a higher baseline cutaneous and gastrointestinal disease activity. The median (IQR) of follow-up was 44.3 months (8.3-80.4). At the end of follow-up, patients with refractory disease had a higher cumulative prednisone dose (15.1 gr [8.6-26.0] vs 9.7 [5.0-16.3], P=0.0005).
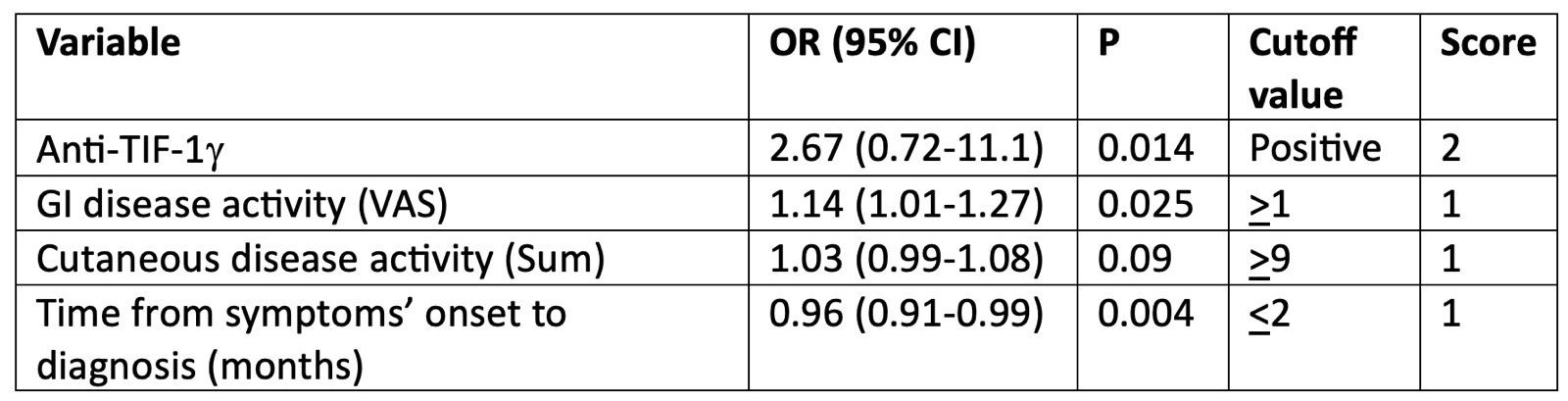
In table 1, we show the OR (95% CI) of the baseline predictive variables, their cutoff points and corresponding numerical values for the creation of the ReMPI.
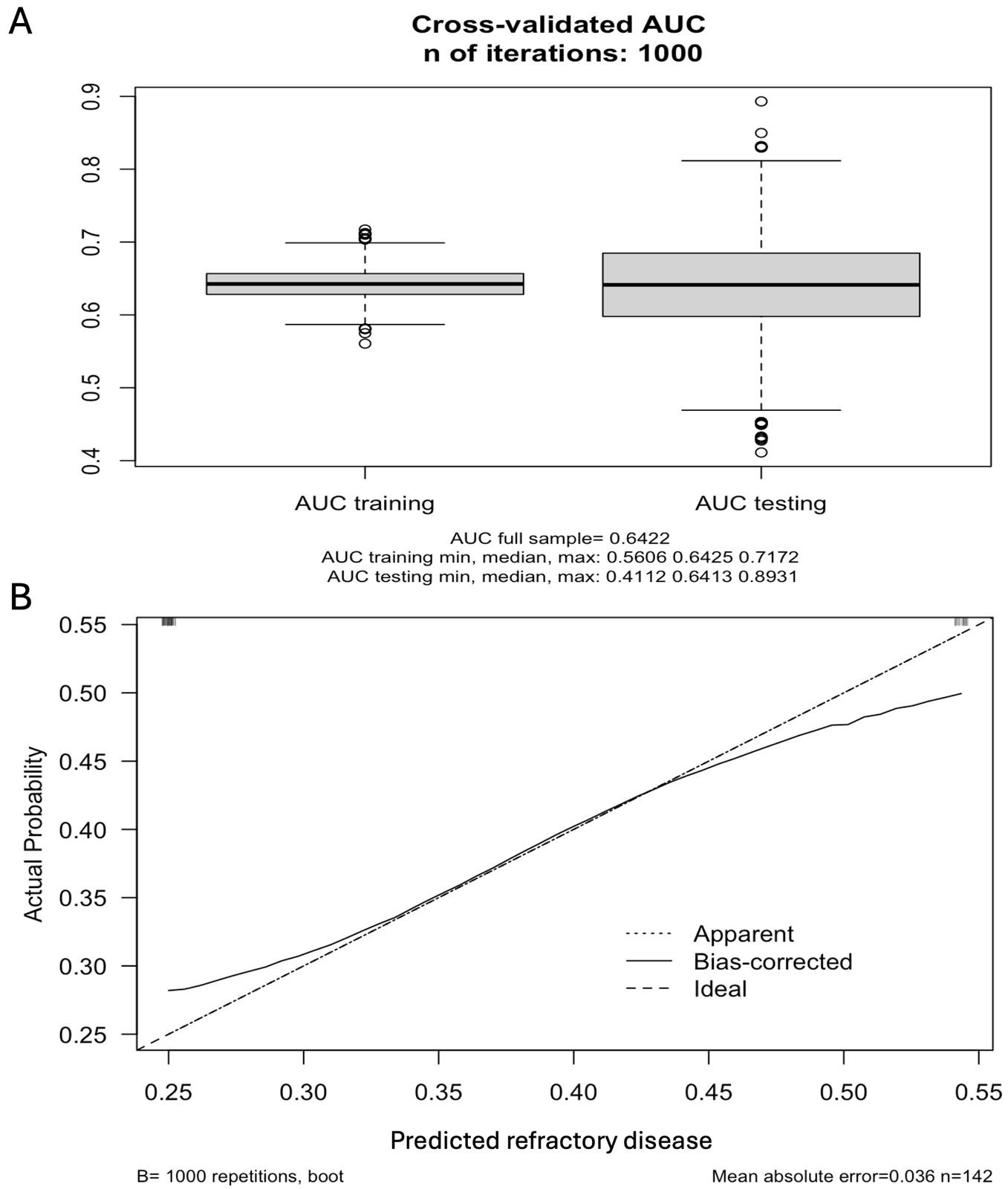
With a cutoff point >1, the ReMPI predicted disease refractoriness with an OR (95% CI) of 3.57 (1.71-7.59), P=0.0006, an optimism-corrected area under de curve of 0.64 and showed a good internal validity and calibration as shown in Figure 1.
Conclusion: The ReMPI is the first index to predict refractory disease in IIM patients. After external validation, the ReMPI may be clinical and easily available tool to identify IIM patients who might benefit from a more aggressive initial immunosuppressive therapy to prevent treatment toxicity, disability and damage accrual.
To cite this abstract in AMA style:
Gaytan Garcia de Alba A, Mejía-Domínguez N, Reyna-Juárez Y, Alcalá-Carmona B, Ostos-prado M, Hernandez Lopez A, Gomez-martin D, Torres Ruiz J. Construction of a Refractory Myositis Predictive Index (ReMPI) in a Cohort of Patients with Idiopathic Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/construction-of-a-refractory-myositis-predictive-index-rempi-in-a-cohort-of-patients-with-idiopathic-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/construction-of-a-refractory-myositis-predictive-index-rempi-in-a-cohort-of-patients-with-idiopathic-inflammatory-myopathies/