Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: People with rheumatic diseases may be at high risk for poor outcomes related to COVID-19; on the other hand, immunomodulatory medications are used as therapy for severe COVID-19. Here, we report a case series of 26 patients with known rheumatic disease who were confirmed as having COVID-19 and compared medication use and other characteristics of hospitalized patients with those who were not hospitalized.
Methods: Established patients being followed at Temple Rheumatology Associates as well as patients admitted to Temple University Hospital in Philadelphia who tested positive for SARS-CoV2 were identified. We analyzed the demographic and clinical characteristics of patients with rheumatic disease and COVID-19 as well as associated outcomes.
Results: Of the patients in our case series, most common rheumatic conditions seen in both hospitalized and non-hospitalized groups were RA and SLE (35%, 23%) (Table 1). The majority of patients in both the hospitalized and non-hospitalized groups were in remission or low disease states (58%).
23% were receiving biologic medications and 20% were on no therapy. The most common therapy among both hospitalized and non-hospitalized patients was HCQ (40%, 50%), with 25% and 33% on HCQ monotherapy, respectively.
The most prevalent comorbidities were obesity (35%), hypertension (46%), COPD/asthma (27%), and diabetes (27%).
Conclusion: We report a case series of 26 patients with rheumatic disease and COVID-19 followed at an academic medical center in a geographic “hot spot.” High numbers of patients who are Black or of Latinx ethnicity in this case series are in line with prior published reports. Our rate of hospitalization (77%) is also relatively high; however, this calculation as well as assessment of frequency of complications is likely confounded by low testing rates in our area for asymptomatic or minimally symptomatic patients, and our baseline number of COVID-19 patients may be much larger.
The most frequent complication in hospitalized patients was hyperinflammatory syndrome (65%), a complication of severe COVID-19 (Table 2); in our center, this was treated aggressively with further immunosuppression such as IL-1 and IL-6 inhibitors and systemic steroids. There was only one death among all included patients. The cause of this discrepancy between severity of illness and death is not clear and may be related to the local rate of infection as well as treatment practices at our center.
In terms of treatment, the most common therapy among our patients was HCQ (42%). Interestingly, no patients were on IL-1, IL-6, IL-17, IL-12/23, CTLA4-Ig, or tsDMARDs. However, absence of evidence is not evidence of absence, and this finding may reflect the social distancing measures being practiced by our patients.
 * No patients were on IL-1, IL-6, IL-17, IL-12/23, CTLA4-Ig, or tsDMARDs.
* No patients were on IL-1, IL-6, IL-17, IL-12/23, CTLA4-Ig, or tsDMARDs.
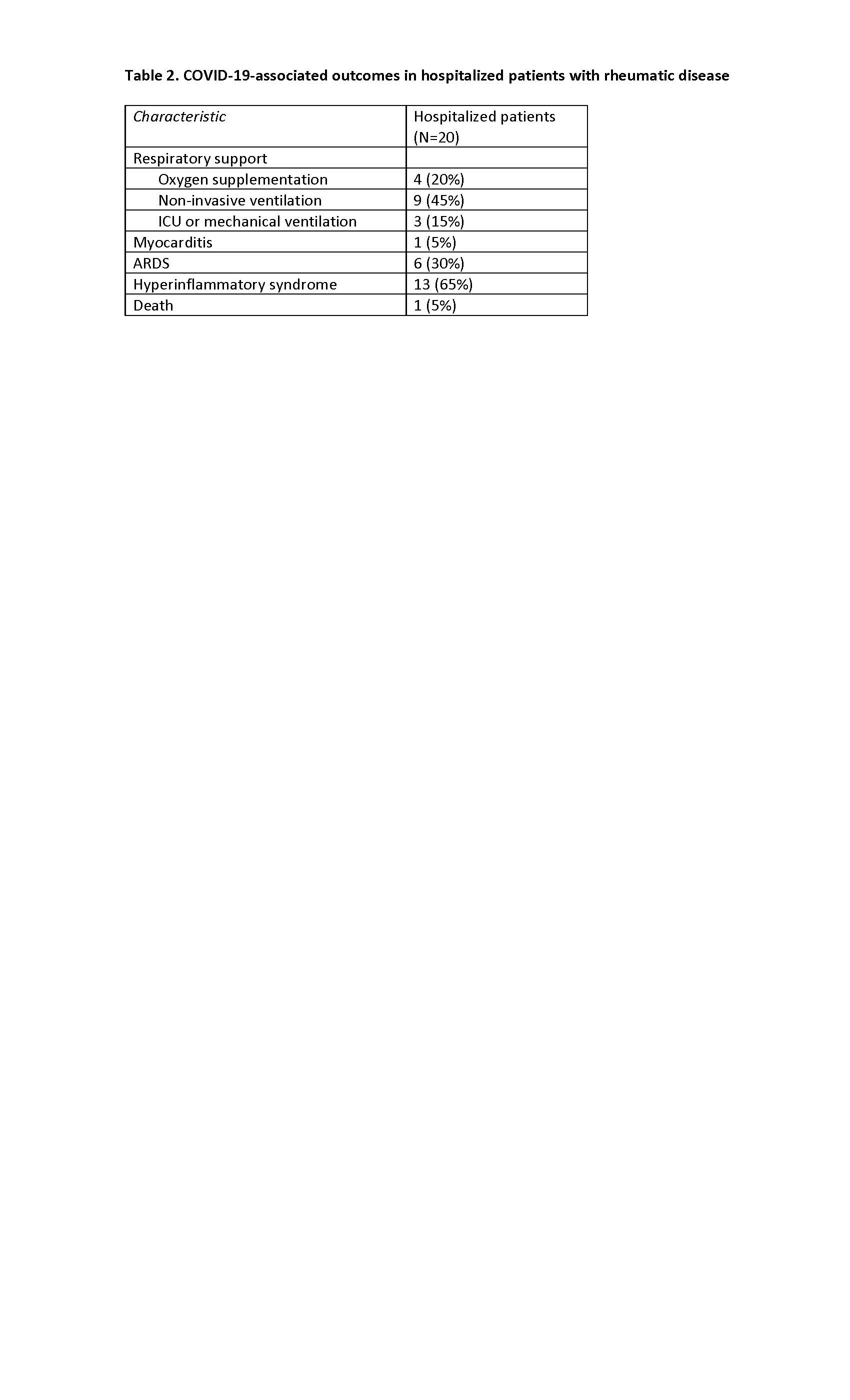 Many hospitalized patients were affected with severe COVID requiring ventilatory support or associated with a hyperinflammatory state.
Many hospitalized patients were affected with severe COVID requiring ventilatory support or associated with a hyperinflammatory state.
To cite this abstract in AMA style:
Buckey T, Jurkowski M, Lu K, Caricchio R, Jayatilleke A. Complications of COVID-19 Infection in Patients with Rheumatic Disease: A Case Series [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/complications-of-covid-19-infection-in-patients-with-rheumatic-disease-a-case-series/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/complications-of-covid-19-infection-in-patients-with-rheumatic-disease-a-case-series/
