Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Pneumonia is a common cause of death not only in the general population but also in patients with rheumatoid arthritis (RA). In particular, patients with RA have an increased risk for pneumonia due to rheumatoid lung disease and the use of some DMARDs. No studies have assessed differences in the management and prognosis of pneumonia in patients with RA compared to the general population. This study aimed to examine the prognosis of pneumonia and its management in patients with RA compared to the general population.
Methods: This study utilized the Diagnosis Procedure Combination database, a nationwide inpatient database in Japan. We reviewed abstract data and medical procedures to identify patients with pneumonia with or without RA between 2014 and 2016. We assessed differences in medical actions: examinations (such as imaging examination, bacteria culture, and antigen testing), interventions (such as oxygen supplementation, use of mechanical ventilation, and ICU admission), and treatment (such as type of antibiotic and duration of antibiotic therapy) between patients with and without RA. We compared the prognosis of pneumonia (mortality, length of hospitalization, aggravation of activities of daily living (ADL), and readmission) between patients with RA and those without RA. We examined the association between RA and pneumonia prognosis using multivariate analysis, adjusting for patients’ background data, comorbidities, and pneumonia severity at admission.
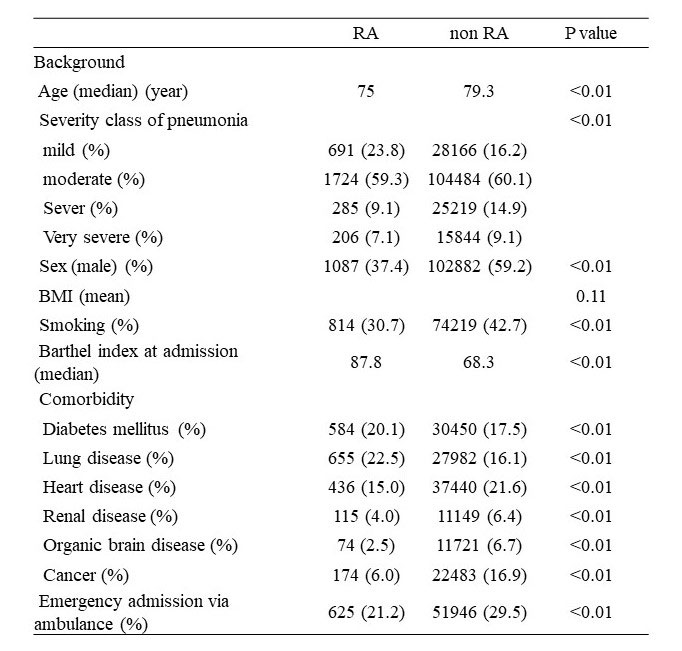
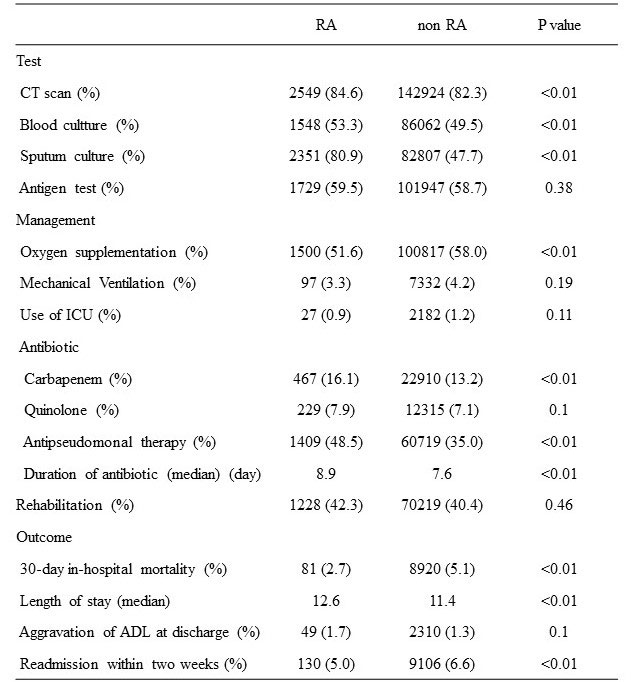
Results: For this study, 178,994 patients from 1,570 hospitals were eligible. Of these patients, 2,951 (1.6%) were diagnosed with RA. The severity of pneumonia in patients WITH RA was mild-to-moderate compared with patients without RA (p< 0.01). Patients with RA had more CT scans performed (84.6% vs 82.3%, p< 0.01) and more sputum culture tests (80.9% vs 47.7%, p< 0.01). Furthermore, broad-spectrum antibiotics (e.g., carbapenem) were frequently administered (16.1% vs 13.2%, p< 0.01) and the antibiotic administration period was slightly longer (8.9 days vs 7.6 days, p< 0.01) in these patients. Patients with RA had lower 30-day in-hospital mortality than those with RA (2.7% vs 5.1%, p< 0.01), but the length of hospital stay was longer (12.6 vs 11.4, p< 0.01). Multiple logistic regression analysis revealed that patients with RA did not have an associated increased risk of in-hospital mortality after adjusting for covariates in each pneumonia severity class (OR 1.36, 95% CI: 0.86-2.14). Lengthened hospitalization period was observed in patients with RA by Cox regression analysis (OR 0.78, 95% CI: 0.75-0.82).
Conclusion: Although pneumonia in patients with RA is not as severe as that in general patients, the rates of examination were high and broad-spectrum and long-term antibiotic treatment were administered more frequently in patients with RA. RA does not affect the prognosis of pneumonia but affects the hospitalization period. It is necessary to consider the implementation of appropriate medical practices according to the severity and the patient background for pneumonia in patients with RA.
To cite this abstract in AMA style:
Uechi E, Fushimi K. Comparison of the Management and Prognosis of Pneumonia in Patients with and Those Without Rheumatoid Arthritis Using the Japanese Diagnosis Procedure Combination Database [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparison-of-the-management-and-prognosis-of-pneumonia-in-patients-with-and-those-without-rheumatoid-arthritis-using-the-japanese-diagnosis-procedure-combination-database/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-the-management-and-prognosis-of-pneumonia-in-patients-with-and-those-without-rheumatoid-arthritis-using-the-japanese-diagnosis-procedure-combination-database/