Session Information
Date: Sunday, November 12, 2023
Title: (0691–0721) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular disease (CVD) has been reported as the most common cause of death in ANCA-associated vasculitis (AAV)1,2. Systemic inflammation, in addition to traditional risk factors such as diabetes mellitus (DM), has been suggested as the main contributor to cardiovascular (CV) events in vasculitis, as there is a well-known association between chronic inflammation and atherosclerosis3.
The aim of this study is to assess the CV risk in patients with vasculitis and DM, and understand whether the risk of CVD in patients with vasculitis is as high as in those with DM.
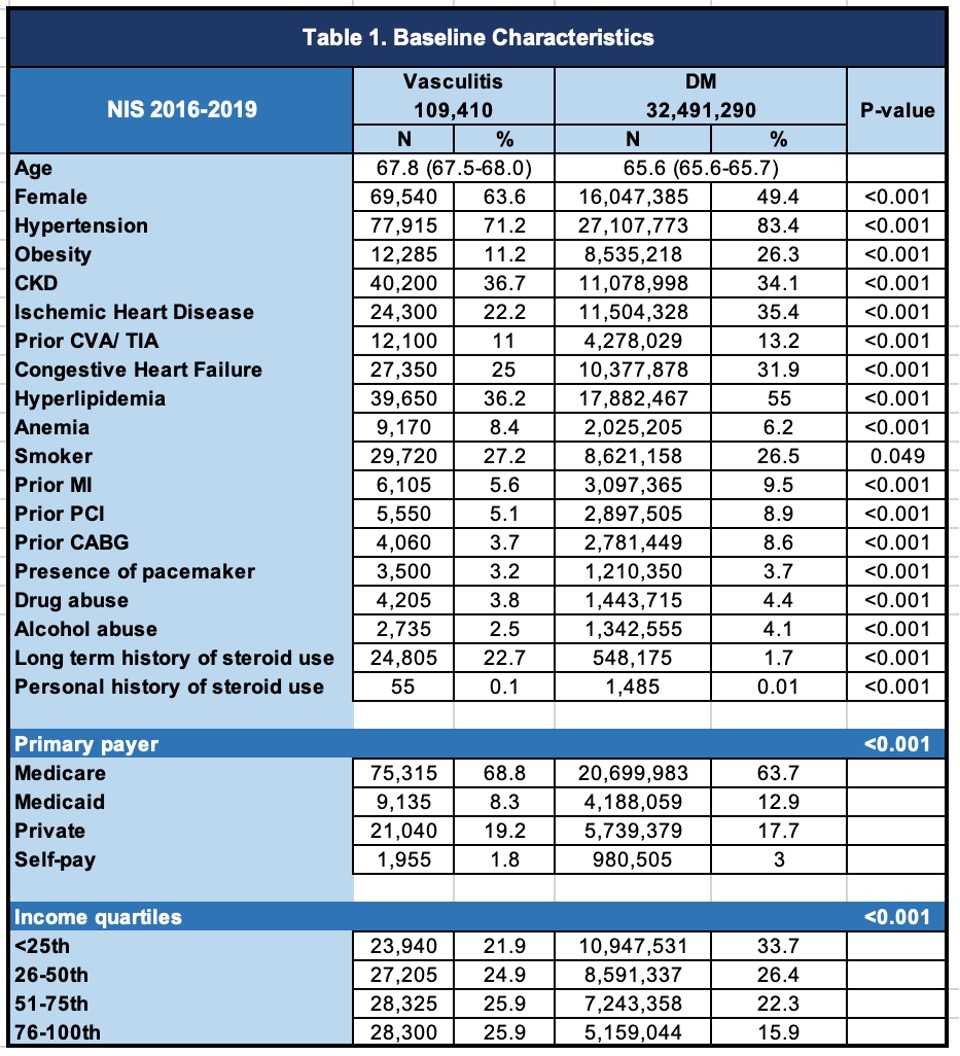
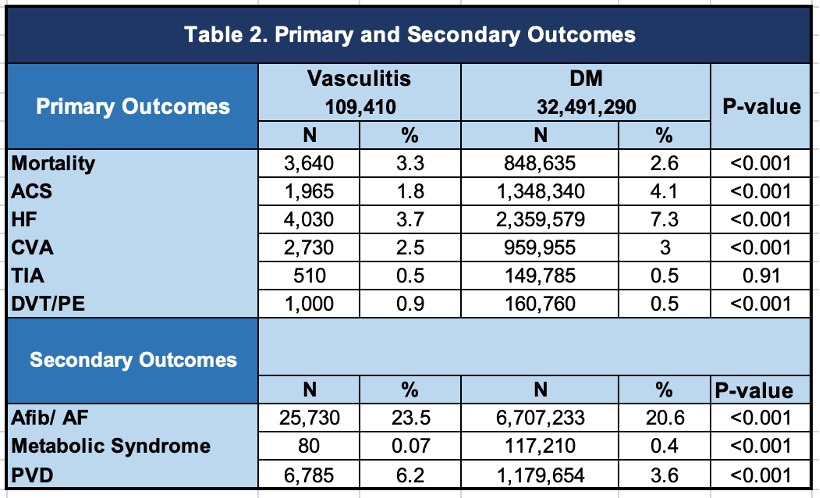
Methods: In this retrospective cohort study, we identified patients with different types of vasculitis without DM based on ICD-10 codes, including large vessel vasculitis (LVV), ANCA-associated vasculitis (AAV), and other vasculitis such as Bechet disease (BD), polyarteritis nodosa (PAN) and cryoglobulinemia. We used the Nationwide Inpatient Sample database (NIS) from 2016 to 2019. We included all-cause mortality, acute coronary syndrome (ACS), cerebrovascular accident (CVA), transient ischemic attack (TIA), and deep venous thrombosis (DVT) or pulmonary embolism (PE) as our primary outcomes. Atrial fibrillation (Afib), atrial flutter (AF), peripheral vascular disease (PVD), and metabolic syndrome were our secondary outcomes. We implemented logistic regression analysis in the univariable and multivariable models. In the multivariable model, we adjusted all outcomes for potential confounders, including age, sex, ethnicity, obesity, anemia, hypertension, renal failure, history of smoking or alcohol abuse, prior history of MI, primary coronary intervention, or coronary artery bypass grafting, coagulopathy, ischemic cardiomyopathy, Elixhauser comorbidity index, hypothyroidism, history of defibrillator or pacemaker, and long-term use of steroids, insurance status and income quartiles. The analysis was done using the STATA software, version 17.0 (MP).
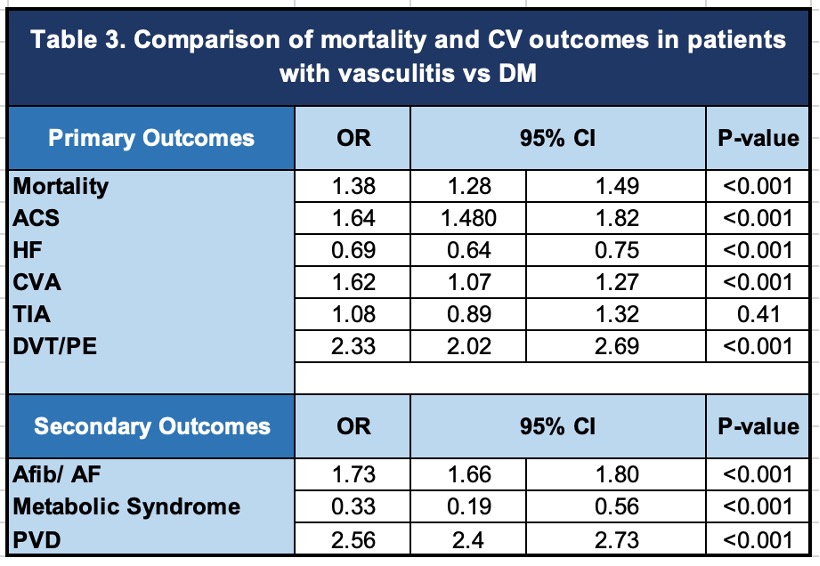
Results: We identified 32,491,290 patients with DM and 109,410 patients with vasculitis without DM, of whom 50,265 (46%) had LVV, 41,220 (37.7%) had AAV, and 13,635 had other vasculitides (12.5%). Our results showed that patients with vasculitis had a higher mortality (OR: 1.38; 95%-CI 1.28-1.49; p-value < 0.001), and increased risk of developing ACS (OR: 1.64; 95%-CI 1.48-1.82; p-value < 0.001), CVA (OR: 1.62; 95%-CI 1.07-1.27; p-value < 0.001), DVT/PE (OR: 2.33; 95%-CI 2.02-2.69; p-value < 0.001), Afib/AF (OR: 1.73; 95%-CI 1.66-1.80; p-value < 0.001), and PVD (OR: 2.56; 95%-CI 2.4-2.73; p-value < 0.001) when compared to patients with DM even after adjusting for potential confounders.
Conclusion: Patients with vasculitis had a higher risk of cardiovascular disease and venous thromboembolism. Our study confirms the high CV risk in patients with vasculitis as highlighted in previous studies, and suggests an even higher risk when compared to patients with DM.
To cite this abstract in AMA style:
Arevalo A, Zala H, Ramirez Gomez A, Ko K. Comparison of the Cardiovascular Risk in Patients with Vasculitis and Diabetes Mellitus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/comparison-of-the-cardiovascular-risk-in-patients-with-vasculitis-and-diabetes-mellitus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-the-cardiovascular-risk-in-patients-with-vasculitis-and-diabetes-mellitus/