Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Lupus nephritis (LN) affects many patients with pediatric systemic lupus erythematosus (pSLE) and is a significant cause of disease morbidity. Inability to achieve remission of LN is associated with worse outcomes. Data from studies of adult patients with combined proliferative plus membranous LN (P/MLN) suggests that this combined subtype may be more refractory to current treatment strategies than isolated proliferative LN (PLN). The possibility that P/MLN may represent a more difficult to treat subtype in the pediatric population has not yet been examined. We aim to assess whether remission occurs less frequently in pediatric P/MLN, compared to pediatric PLN.
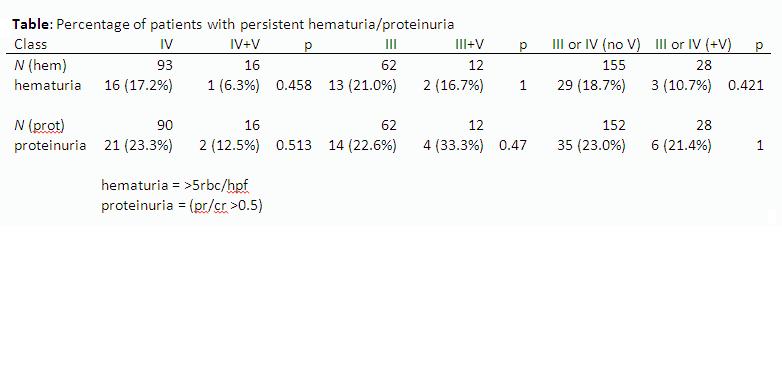
Methods: CARRA Registry data was obtained for 320 subjects with pSLE (age at onset <18 years) and LN; LN was diagnosed by renal biopsy and categorized according to ISN/RPS classification criteria. Remission of proteinuria was defined as protein/creatinine ratio < 0.5. Remission of hematuria was defined as < 6 RBC/hpf on urinalysis. These cutoffs were determined by the available clinical data from the CARRA registry. Remission was assessed at the most recent CARRA registry visit gathered ≥ 6 months after diagnostic kidney biopsy. Medication exposure data, non-renal disease characteristics, and demographic data were also assessed. Comparison of these data between subjects with P/MLN and subjects with PLN was conducted.
Results: A total 184 subjects had PLN (class III or class IV) and a total of 38 subjects had M/PLN (class III+V or class IV+V). No significant difference in proportion of subjects with remission in either proteinuria or hematuria was found between groups with and without membranous disease. (See Table). Estimated GFR less than 90 ml/min/1.73m2, indicating renal insufficiency, was found in 6.1 and 16.1% of subjects with PLN and P/MLN respectively, approaching statistical significance (p=0.07). Exposure rates to mycophenolate, cyclophosphamide, and rituximab were similar between groups. Patients in PLN and M/PLN groups were similar with respect to SLEDAI scores at last study visit, age of SLE onset, gender distribution, and ANA positivity. Subjects with class IV+V were significantly older at first renal biopsy compared to subjects with class IV (mean age 14.83 vs. 12.71, p=0.005), although this trend was not significant for comparison of subjects with class III vs. class III+V.
Conclusion: CARRA registry subjects with P/MLN and PLN have similar rates of remission for hematuria and proteinuria assessed at the last CARRA registry visit. There was a trend for the P/MLN group to have more renal insufficiency. This study was limited by its cross-sectional, retrospective design, and future longitudinal prospective studies will be useful in further assessing the relationship between renal histology findings and response of pediatric LN to treatment.
Disclosure:
A. Boneparth,
None;
N. T. Ilowite,
None;
T. CARRA Registry Investigators,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-remission-rates-for-pediatric-membranous-plus-proliferative-lupus-nephritis-versus-isolated-proliferative-lupus-nephritis-an-analysis-of-the-childhood-arthritis-and-rheumatism-research/