Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Almost all patients with SLE experience joint problems and arthritis, 12% suffer permanent joint damage. The wide variability in SLE arthritis and the limitations of existing assessment tools make it difficult to identify musculoskeletal involvement in clinical care and clinical trials. Identifying lupus arthritis based on physical exam remains challenging. Clinicians need a robust, easy-to-use imaging technique to diagnose and monitor arthritis in SLE. Ultrasound (US) and magnetic resonance (MRI) allow for more objective assessments but are plagued by operator dependence and high cost. With the support of a DoD award, we are developing a prototype imaging system that uses lasers and light detectors to evaluate finger joints in SLE. Here we describe preliminary data on comparisons between optical imaging and US evaluations of affected and unaffected proximal interphalangeal (PIP) joints.
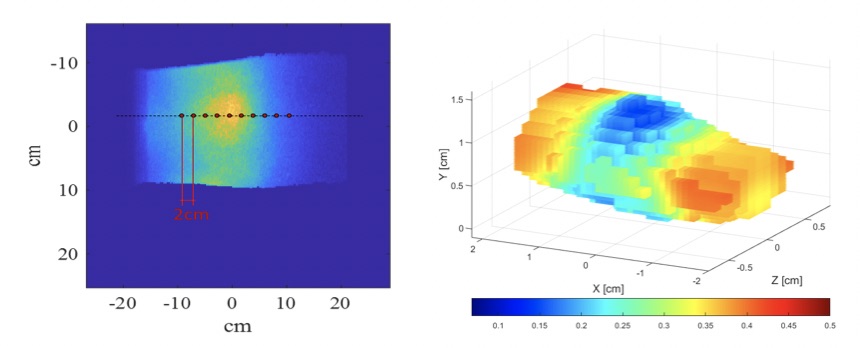
Methods: Fifteen SLE patients were evaluated, 8 PIP joints (bilateral PIP 2-5)/patient were imaged, with a total of 120 images. A systematic multiplanar grey-scale (GS) and power doppler (PD) examination of PIP joints was performed using the Outcome Measures in Rheumatology (OMERACT) consensus definitions for joint pathologies, and a combined PDGS score was calculated. Immediately after the US, joints were examined using optical imaging. The instrumentation uses a 670nm, 8mW laser with a 1 mm diameter beam modulated at 300 MHz as light source. The laser beam is focused on the dorsal surface of each finger and scans across the PIP joints (as shown in Figure 1, left). The transmitted light is collected by an intensified charge-coupled device camera and the absorption and scattering distributions inside the finger are reconstructed (Fig.1 shows absorption) using a radiative transfer equation model.
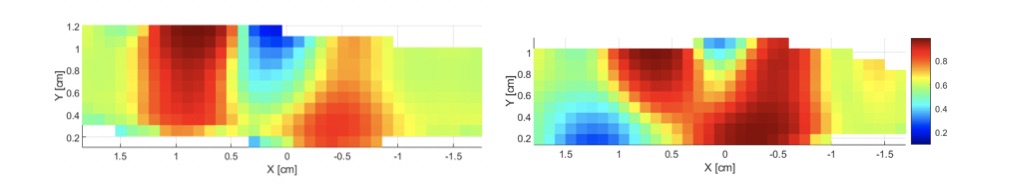
Results: The PDGS scored 34 joints 0, 44 – 1, 20 – 2 and 22 – 3. The absorption and scattering data were obtained from the reconstructed images. Figure 2 shows a cross section through an unaffected joint (PDGS=0) on the left and an affected joint (PDGS=3) on the right. The average absorption coefficient of joints with PDGS = 0 or 1 was 0.52±0.19 cm-1, while joints with PDGS = 2 or 3 the absorption was 0.60±0.19 cm-1, p < 0.05. Similarly, we found that the difference in the scattering coefficients between the two groups was also statistically significant (10.8±1.9 cm-1 versus 11.8±2.1 cm-1, p< 0.01).
Conclusion: Optical imaging correlated with PDGS findings in 120 evaluated lupus arthritis PIP joints. Further examination of SLE arthritis using the new US OMERACT criteria that includes a tenosynovitis score and MRI will allow for better definitions of PIP arthritis and improve the correlations with optical imaging. The system, which could take the form of an ergonomic glove, will allow the investigators to image lupus arthritis, both in the office and at home, to diagnose and monitor arthritis progress. The goal is to create a portable, wearable, imaging device that permits real-time monitoring of SLE arthritis to improve patient care and outcomes.
To cite this abstract in AMA style:
Tang W, Marone A, Khalili L, Wang X, Murray S, Inzerillo S, Bardien M, Gaikwad V, Kim S, Geraldino-Pardilla L, Hielscher A, Askanase A. Comparison of Optical and Ultrasound Imaging in Lupus Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/comparison-of-optical-and-ultrasound-imaging-in-lupus-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-optical-and-ultrasound-imaging-in-lupus-arthritis/