Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Around 2-12% of patients who undergo open thoracic aortic aneurysm repair are incidentally found to have aortitis on pathology. There is no standardized approach to the post-operative care of patients with incidentally-found aortitis nor extensive data on post-operative and long-term outcomes. A better understanding of the risk for recurrent vascular disease and surgical complications in this population could inform clinical surveillance and treatment. This study compared immediate post-operative and long-term outcomes between patients with pathology-diagnosed aortitis and those with non-inflammatory aortic aneurysms after undergoing open thoracic aortic aneurysm repair.
Methods: This is a single-center matched cohort study. Patients with aortitis were identified by histopathology following open thoracic aortic aneurysm repair in the University of Pennsylvania Health System between 2007 and 2017 and lacked any evidence of infection or known prior diagnosis of rheumatic disease. Two comparators who lacked significant inflammation on pathology were matched to each aortitis case by year of surgical repair. Outcomes included length of hospital stay, surgical complications, formation of new vascular abnormalities on CT/MRI imaging, and death. Differences between groups were compared using conditional logistic, Cox proportional hazards, or conditional Poisson regression models accounting for matching.
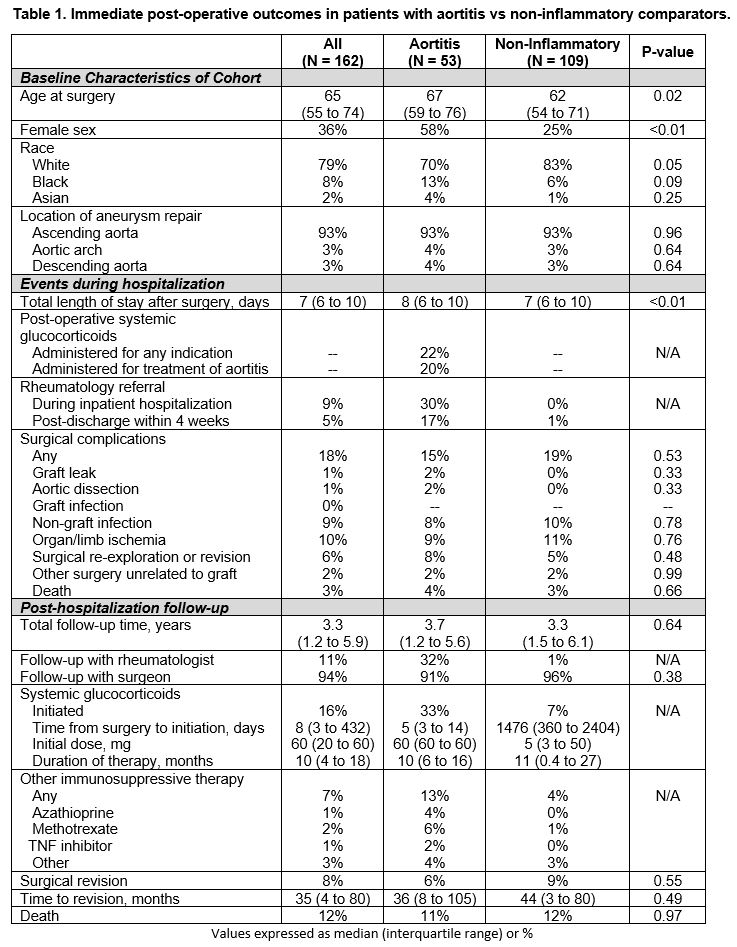
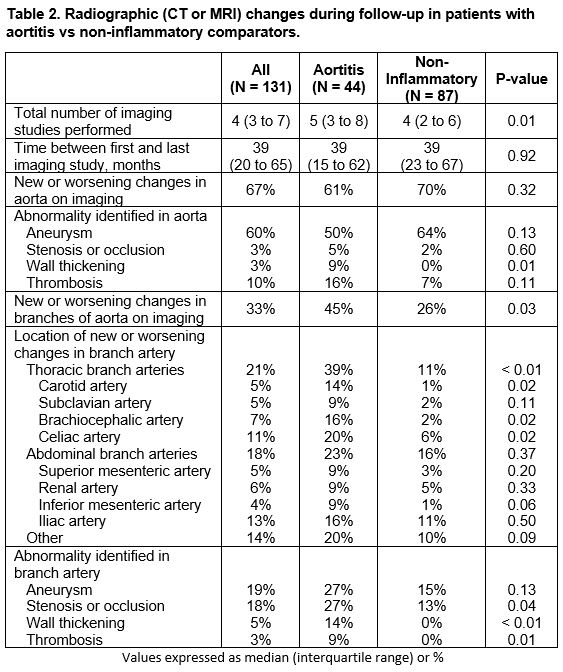
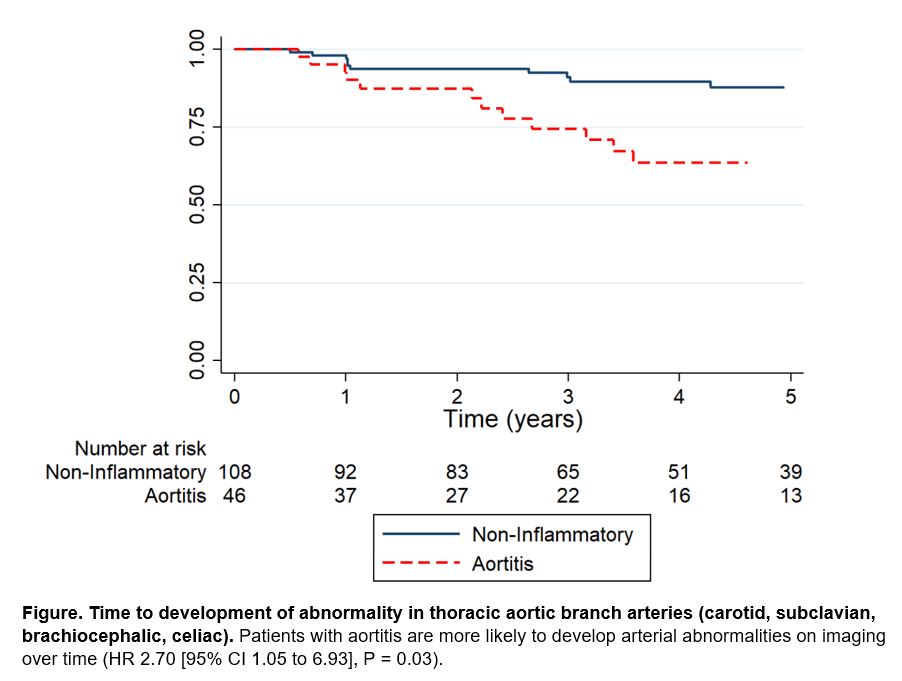
Results: For the analysis, 162 patients were included: 53 patients with aortitis and 109 matched comparators with similar follow-up time between groups (median follow-up 3.7 vs 3.3 years) (Table 1). Aortitis patients were more likely to be older, female and less likely to have a history of coronary artery disease. 93% of each group had an ascending thoracic aortic aneurysm that was repaired (Table 1). Patients with aortitis had a significantly longer hospital length of stay even after adjusting for perioperative glucocorticoid use and referral to rheumatology (adjusted IRR 1.35 (1.19 to 1.53), P < 0.01). There was no difference in rates of post-operative complications or surgical revision between groups (Table 1). On long-term surveillance imaging, no difference was seen in new or worsening aortic aneurysms between groups, but there were significantly more vascular abnormalities in the thoracic aortic branch arteries (carotid, subclavian, brachiocephalic, and celiac arteries) in the aortitis group (39% vs. 11%, P < 0.01)(Table 2, Figure).
Conclusion: Among patients who underwent open surgical repair of a thoracic aortic aneurysm, patients with incidentally-discovered aortitis were more likely than non-inflammatory comparators to have a longer hospital length of stay and develop vascular anomalies in major aortic branch arteries. The higher rate of arterial abnormalities in patients with aortitis may reflect ongoing inflammatory changes from an underlying vasculitic process and suggest that more frequent surveillance imaging and involvement of a rheumatologist are needed in the long-term care of these patients.
To cite this abstract in AMA style:
Mayer A, Sperry A, Quimson L, Rhee R. Comparison of Immediate Post-Operative and Long-Term Outcomes in Aortitis and Non-Inflammatory Thoracic Aortic Aneurysms Undergoing Open Surgical Repair [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/comparison-of-immediate-post-operative-and-long-term-outcomes-in-aortitis-and-non-inflammatory-thoracic-aortic-aneurysms-undergoing-open-surgical-repair/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-immediate-post-operative-and-long-term-outcomes-in-aortitis-and-non-inflammatory-thoracic-aortic-aneurysms-undergoing-open-surgical-repair/