Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: The COVID-19 pandemic has brought uncertainties to the rheumatological practice, and despite the large number of publications to date, many questions remain unanswered. One of the unmet needs is related to the differential risk among the immune mediated rheumatic diseases (IMRD), mainly related to the severity COVID-19 outcomes.
The aim of this study was to compare COVID-19 outcomes among patients with Systemic Lupus Erythematosus (SLE), Rheumatoid Arthritis (RA) and Spondyloarthritis (SpA) in a cohort of Brazilian patients and the main risk factors associated.
Methods: We performed a cross-sectional analysis from the ReumaCoV-Brasil registry comparing the moderate/ severe forms, including hospitalization, intensive care unit (ICU) admission, mechanical ventilation (MV) and death, in patients with RA, SLE and SpA and COVID-19. COVID-19 diagnosis was defined as clinical symptoms and lab test confirmation (RT-PCR and/ or serology against SARS-CoV-2). Demographic and clinical data, as well as details on COVID-19 management and endpoints were collected on the REDCap database. Specific and international classification criteria were used to define each IMRD of this study. This study was registered at the Brazilian Registry of Clinical Trials—REBEC, RBR-33YTQC.
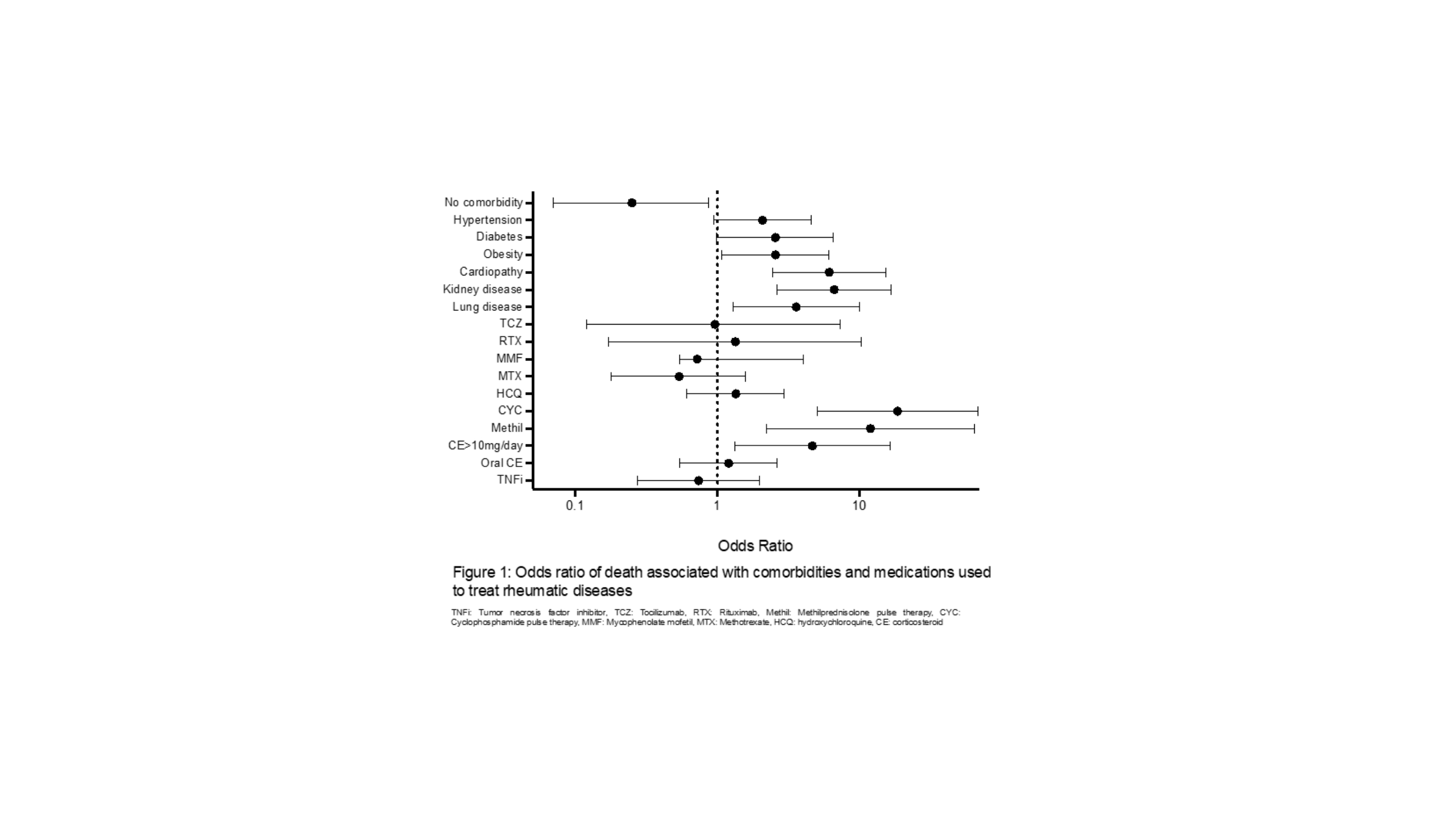
Results: From May 20th, 2020 to Jan 24th, 2021, a total of 751 patients were included, of whom 317 with SLE (42.2%), 269 with RA (35.8%) and 165 with SpA (22.0%). Most of patients were female (81.6%) with mean age was 46.7 (13.5) years. The main comorbidity was hypertension (36.6%). Regarding the symptoms of COVID-19, patients with RA reported a higher frequency of arthralgia than the other groups (35.3% vs. 23.0% and 21%; p=0.001, respectively) and longer symptoms duration (15.5±10.7 days vs. 12.1±8.8 days and 13.1±9.9 days, p< 0.001, respectively). The COVID-19 endpoints were quite similar among groups, including hospitalization, ICU admission, MV and mortality rate (Table 1). Analyzing the whole group, older age was significantly associated with all outcomes, as well current oral corticosteroids dosage above 10mg/day and cardiopathy. On the other hand, absence of any comorbidity played a protective role for all the outcomes. After multiple adjustments, the risk factors associated with death were age (OR=1.03; 95%CI 1.004-1.09, p=0.027) and have no kidney disease (OR = 0.150; 95%CI 0.04-0.45, p=0.0001) (Figure 1).
Conclusion: Although no differences have been observed regarding COVID-19 outcomes among patients with SLE, RA and SpA, some risk factors associated with death, hospitalization, IUC admission and MV are directly related to DMARDs, particularly current corticosteroids. However, it is important to note that traditional risk factors are more related to unfavorable COVID-19 than underlying IMRD, especially older age and comorbidities.
To cite this abstract in AMA style:
Marques C, Reis A, Kakehasi A, Neto E, Pinheiro M, Pileggi G, Ferreira G, Mota L, Andre Monticielo O, Ribeiro S, Omura F, Marinho A, Ribeiro F, Rocha Jr L, Martins A, Yazbek M, Souza M, Sacilotto N, Shinjo S, Valadares L, Silva A, de Brito D, de Souza V, Costa C, Studart S, Ximenes A, Xavier R. Comparison of Hospitalization and Mortality Rate in Patients with Different Rheumatic Diseases: A Brazilian Registry Cross-Sectional Analysis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/comparison-of-hospitalization-and-mortality-rate-in-patients-with-different-rheumatic-diseases-a-brazilian-registry-cross-sectional-analysis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-hospitalization-and-mortality-rate-in-patients-with-different-rheumatic-diseases-a-brazilian-registry-cross-sectional-analysis/