Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Quantifying comorbidities contribution to disability and mortality is important for assessing prognosis and standardizing cohorts in rheumatic disease research. A comorbidity index has been developed specifically for individuals with rheumatic diseases. We compared the Rheumatic Diseases Comorbidity Index (RDCI) with the Charlson-Deyo index (CDI) and Functional Comorbidity Index (FCI) using a nationwide cohort of RA patients.
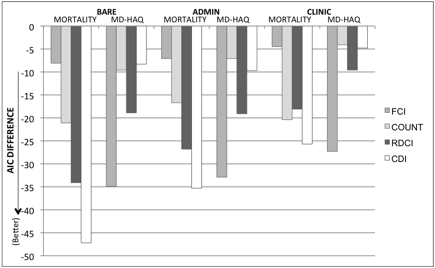
Methods: The RDCI, range 0-9, combines 11 comorbidities: lung disease, hypertension, MI, stroke, heart disease, cancer, fracture, diabetes, depression, GI problem and ulcer. The predictive value of the RDCI, CDI, FCI, and a generic comorbidity count (COUNT) for outcomes of functional disability and mortality were tested in the Veterans Affairs RA registry by access to administrative ICD9 diagnosis codes. Functional disability was measured by MD-HAQ. Comorbidity indices were fixed at baseline values and patient visits were limited to first visits within each of twenty-one six-month phases from January 2003 to March 2013. Best fit via Cox proportional hazard for mortality and Generalized Estimating Equations for disability models was determined by the Akaike Information Criterion (AIC) where a lower AIC signifies a better model fit. Indices were compared in three models: a bare model [age, sex, and race]; an admin model [bare+ visit frequency, BMI, prednisone, and MTX]; and clinic model [admin+ ESR, nodules, RF+, and patient activity scale].
Results: Each index improved the fit of all models (see Figure). Comorbidity indices decreased AIC most in the bare model and least in the clinic model. CDI decreased AIC most in the mortality analysis while performing worst in MD-HAQ. FCI decreased AIC the most in MD-HAQ analysis but performed worst in mortality. RDCI performed well in both mortality and MD-HAQ analysis.
Conclusion: The RDCI quantifies the contribution of comorbidity to both MD-HAQ and mortality well, while other indices were better predictors of only one outcome. In the first study that compares comorbidity indices with administrative data such as ICD9 codes, RDCI performed well and shows promise for future use in observational studies obtaining data from electronic medical records. Furthermore, we demonstrate when choosing a comorbidity index, the outcome of interest and the variables within the model should guide index selection.
Disclosure:
B. R. England,
None;
H. Sayles,
None;
T. R. Mikuls,
None;
D. S. Johnson,
None;
K. Michaud,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-comorbidity-indexes-in-a-clinical-and-administrative-rheumatoid-arthritis-cohort-a-case-for-the-rheumatic-diseases-comorbidity-index/