Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The value of non-invasive vascular imaging for cardiovascular (CV) risk stratification of patients with inflammatory rheumatic diseases is unclear. Measures of atherosclerosis including coronary artery calcification score (CACS) on computerized tomography (CT) scan and both total plaque area (TPA) and carotid intima-media thickness (cIMT) by carotid ultrasound (US) have been reported to improve risk stratification beyond the Framingham Risk Score (FRS). We determined the ability of CACS and US to correctly identify high CV risk patients with inflammatory rheumatic diseases.
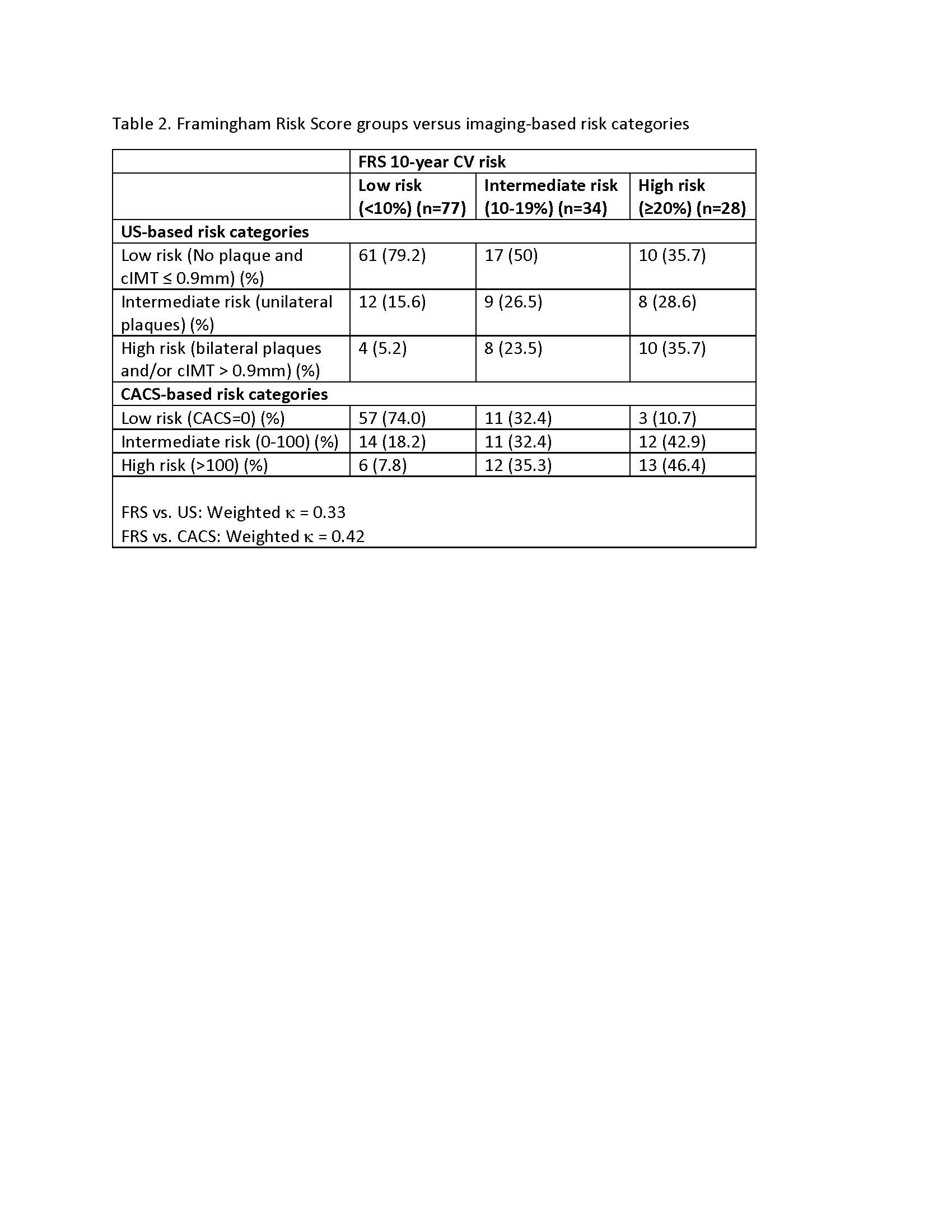
Methods: In this cross-sectional study, patients with ankylosing spondylitis (AS), psoriatic arthritis (PsA) and rheumatoid arthritis (RA), who had no history of CV disease, underwent assessment of CV risk factors from July 2017 to March 2019 in a Cardio-Rheumatology clinic. CACS, cIMT and TPA were measured. The correlation between CACS and cIMT, between CACS and TPA, and between cIMT and TPA was assessed by Pearson correlation coefficient. Based on the FRS, patients were classified into low (< 10%), intermediate (10-20%) and high risk categories ( >20%). Risk categories for US were defined as low (zero plaque and cIMT< 0.9mm), intermediate (unilateral plaque) and high risk (cIMT >0.9mm and/or bilateral plaques). CACS risk categories were defined as low (CACS=0), intermediate (0-100) and high risk ( >100). The weighted Kappa statistic was used to assess agreement between score categories.
Results: 139 patients with RA (49.6%), PsA (37.4%) and AS (12.9%) were assessed (mean age 61.2 ± 10.9 years, 66.9% female) (Table 1). CACS correlated moderately with TPA (r=0.42, p< 0.0001), while there was very weak correlation between CACS and cIMT (r=0.08), and between TPA and cIMT (r=0.14). 29.7% and 16.2% of patients classified into the low and intermediate risk categories based on the FRS had significant atherosclerosis in the carotid (TPA >0) and coronary arteries (CACS >100), respectively (Table 2). 50% of patients in the FRS intermediate risk category were reclassified into an US low risk group, while 35.7% of patients in the FRS high risk category were reclassified into an US low risk group. Importantly, when comparing US and CACS risk categories, 54% of patients in the intermediate CACS risk category were reclassified into a low risk US group (Table 3). There was generally good agreement between the FRS and CACS risk categories in stratifying low and high risk patients, while stratification among intermediate risk patients was poor. Overall, agreement between FRS and US (weighted k = 0.33), CACS and US (weighted k = 0.39), and FRS and CACS (weighted k = 0.42) risk categories was fair to moderate.
Conclusion: There is a moderate agreement between non-invasive carotid vascular and coronary calcium imaging in assessment of atherosclerosis burden in patients with IRDs. The results of the study highlight potential added value of using CACS and TPA in combination with traditional risk scores to improve CV risk stratification.
To cite this abstract in AMA style:
Colaco K, Nguyen E, Akhtari S, Harvey P, Eder L. Comparison of Carotid Ultrasound and Coronary Artery Calcium Score in Cardiovascular Risk Stratification of Patients with Inflammatory Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparison-of-carotid-ultrasound-and-coronary-artery-calcium-score-in-cardiovascular-risk-stratification-of-patients-with-inflammatory-rheumatic-diseases/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-carotid-ultrasound-and-coronary-artery-calcium-score-in-cardiovascular-risk-stratification-of-patients-with-inflammatory-rheumatic-diseases/