Session Information
Date: Sunday, October 26, 2025
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Inflammatory back pain (IBP) is very relevant for identifying patients at risk of axial spondyloarthritis (axSpA). Mounting evidence has indicated substantial variability in sensitivity and specificity among different methods of IBP assessment (1). The aim of this study is to evaluate the concordance and correlation between physician-based ASAS IBP criteria and self-reported IBP, comparing each against expert clinical judgement in a prospective cohort of patients with chronic low back pain.
Methods: A prospective, observational study was conducted at a tertiary hospital (July 2021- October 2023). Patients aged 18–40 years with chronic back pain (≥ 3 months) who underwent spine magnetic resonance imaging (MRI) requested by non-rheumatology specialists were enrolled, and completed a questionnaire capturing variables relevant to axSpA, including characteristics of IBP. Within two weeks, patients underwent a rheumatology evaluation. IBP was evaluated independently using three different approaches: physician-assessed ASAS IBP criteria as a checklist (ASAS-IBP-phy), self-reported ASAS IBP questionnaire (ASAS-IBP-self), and the rheumatologist’s clinical judgement (IBP-rheumatologist). ASAS-IBP-phy and ASAS-IBP-self were evaluated through structured questionnaires completed by the physician and the patient, respectively ,while IBP-rheumatologist relied exclusively on the clinician’s global assessment. Cohen’s and Fleiss’ kappa statistics, along with tetrachoric correlation, assessed the agreement among these methods.
Results: Among 268 enrolled patients, mean age was 35.6 years (SD 5.6), with 149 (55.6%) females. Mean duration of symptoms was 5.1 years (SD 4.6), and 64.2% had symptom duration greater than two years. ASAS-IBP criteria were positive in 79 (29.5%) patients by rheumatologist checklist evaluation (ASAS-IBP-phy), and 82 (30.6%) through self-report (ASAS-IBP-self). Clinical judgement by rheumatologist identified IBP in 54 (20.1%) patients. Among patients with axSpA (n = 8), 7 (87.5%) presented IBP according to the rheumatologist, and among those without axSpA (n = 260), 47 (18.1%) did. 32 patients (11.9%) fulfilled IBP criteria across all three methods (Figure 1). Agreement between physician-based and self-reported IBP criteria was moderate (kappa = 0.42, p < 0.001) with a strong tetrachoric correlation (rt=0.63) (Figure 2). ASAS-IBP-phy showed substantial agreement with IBP according to rheumatologist clinical judgement (kappa = 0.69, p < 0.001), and a very strong tetrachoric correlation (rt=0.93). In contrast, agreement between ASAS-IBP-self and clinical IBP assessment was fair (kappa = 0.34, p < 0.001), with moderate tetrachoric correlation (rt=0.57). Fleiss' kappa for overall agreement among the three assessment methods was 0.31 (p < 0.001).
Conclusion: In this cohort, physician-based ASAS IBP criteria showed higher concordance and correlation with rheumatologist clinical judgement than self-reported criteria. Given these results, clinician-led evaluation should be prioritized when identifying IBP in clinical and research contexts, with cautious interpretation of self-reported data, particularly in remote or digital healthcare settings.
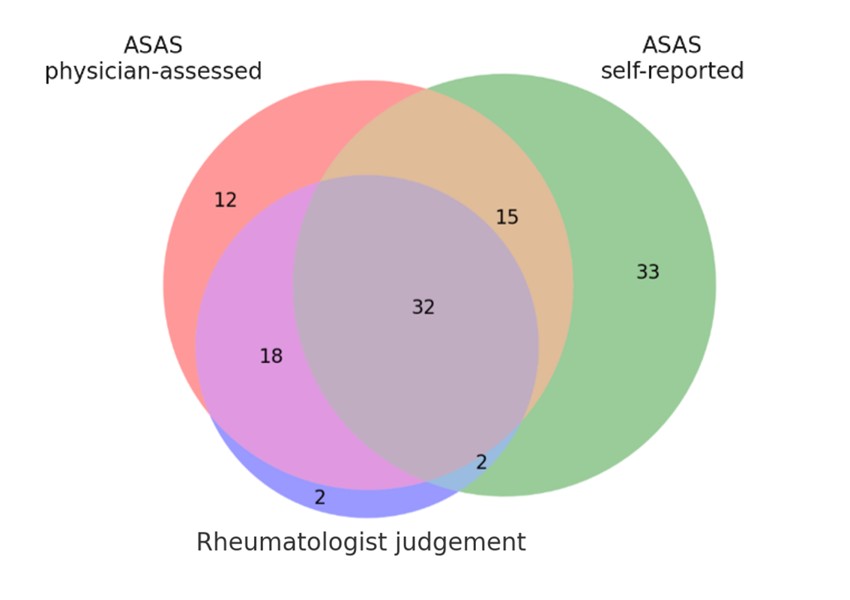 Figure 1. Number of patients with IBP according to each method of assessment
Figure 1. Number of patients with IBP according to each method of assessment
.jpg) Figure 2. Correlation between IBP assessment methods
Figure 2. Correlation between IBP assessment methods
To cite this abstract in AMA style:
Benavent D, Tapia M, Bernabeu D, Muley V, Juárez M, Plasencia-Rodríguez C, Balsa A, Navarro-Compan V. Comparing Perspectives of Physician-Assessed and Self-Reported Inflammatory Back Pain: Insights from the SHERPAS Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/comparing-perspectives-of-physician-assessed-and-self-reported-inflammatory-back-pain-insights-from-the-sherpas-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-perspectives-of-physician-assessed-and-self-reported-inflammatory-back-pain-insights-from-the-sherpas-cohort/
