Session Information
Date: Saturday, November 16, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: 18F-fluoro-deoxyglucose (FDG) is the current standard among radiotracers for PET/CT imaging of large vessel vasculitis (LVV) in giant cell arteritis (GCA), but its performance is influenced by glucocorticoids. We aimed to compare 68Ga-HA-DOTATATE (DOTA), a somatostatin analogue, to FDG for LVV detection using PET/CT in patients with active GCA.
Methods: In this pilot study, 8 active GCA patients (with disease confirmation by either temporal artery biopsy or positive large vessel imaging) who had initiated glucocorticoids within 2 weeks of enrolment were prospectively consented and scanned with both FDG PET/CT and 68Ga-HA-DOTATATE PET/CT. Images were reviewed by 2 experienced Nuclear Medicine physicians. Tracer uptake was assessed by visual scoring (compared to liver) and semi-quantitatively in 8 vascular territories (thoracic and abdominal aorta, bilateral subclavian, vertebral, carotid, femoral/iliac, temporal and coronary arteries) using SUVmax. Target-background ratios (TBR) were calculated using both right atrium (RA) mean (TBRRA) and liver mean (TBRliver) as comparators. Index vessel was defined as the vessel with the greatest tracer uptake in each participant. DOTA and FDG TBR’s in individual vascular territories and index vessels were compared using Wilcoxon signed rank test. P< 0.05 was considered statistically significant.
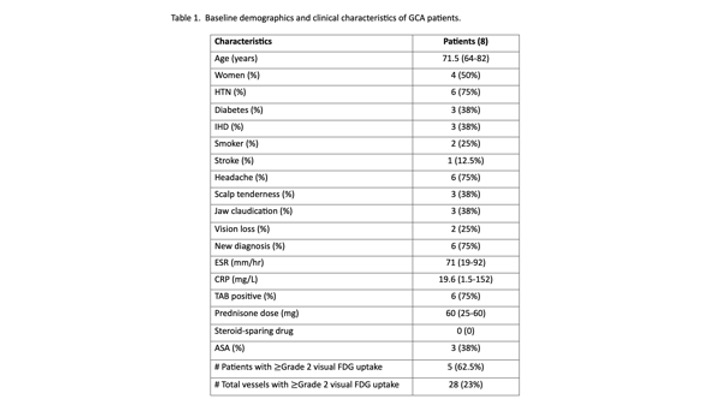
Results: Of 8 enrolled patients, the median age was 71.5 years (range 64-82), and 4 (50%) were women. See Table 1 for baseline characteristics. Five of 8 (62.5%) FDG scans had >= grade 2 visual uptake in the large vessels, consistent with active LVV. Tracer uptake could be detected semi-quantitatively in the medium-large arteries in both FDG and DOTA scans. DOTA identified a different index vessel from FDG in 4/8 (50%) patients.
The FDG median SUVmax values were significantly higher than DOTA median SUVmax values in every individual vascular territory (p< =0.025 for all comparisons), as was the FDG median RA SUVmean [1.85 in FDG vs 0.35 in DOTA, z=2.52, p=0.012]. Due to very low blood pool activity, calculated DOTA median TBRRA values were significantly higher in every individual vascular territory as compared to FDG (p< = 0.025 for all comparisons), and the DOTA median Index Vessel TBRRA was significantly higher than the FDG median Index Vessel [5.08 vs 1.805, z=-2.38, p=0.017.)
In contrast, the FDG median Liver SUVmean was significantly lower as compared to DOTA [2.38 vs 7.88, z=2.52, p=0.012]. Correspondingly, DOTA median TBRliver values were significantly lower in every vascular territory as compared to FDG (p=0.012 all comparisons), as was DOTA median Index Vessel TBRliver as compared to FDG [0.242 vs 1.39, z=-2.52 p=0.012.)
Conclusion: 68Ga-HA-DOTATATE uptake can be detected in the aorta and medium branch vessels, including temporal and coronary arteries, of patients with active GCA who have started glucocorticoids. The distribution of DOTA uptake differs from that of FDG, with significantly lower blood pool and higher liver uptake, corresponding to higher vascular TBRRA values and lower TBRliver values. Additional work is needed to determine the best method of quantifying vascular DOTA uptake in GCA.
To cite this abstract in AMA style:
Clifford A, Abele J, Hung R, Raggi P, Wuest F, Andersson J, Yacyshyn E, Lenza E, Jickling G, Cohen Tervaert J. Comparing Large Vessel Uptake of 68Ga-HA-DOTATATE to 18F-FDG Using PET/CT Imaging in Patients with Active Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/comparing-large-vessel-uptake-of-68ga-ha-dotatate-to-18f-fdg-using-pet-ct-imaging-in-patients-with-active-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-large-vessel-uptake-of-68ga-ha-dotatate-to-18f-fdg-using-pet-ct-imaging-in-patients-with-active-giant-cell-arteritis/