Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Antiphospholipid antibody syndrome (APS) is an autoimmune hypercoagulable state caused by antiphospholipid antibodies (aPL) which represent a diagnostic criterion and underlie significant comorbidities in patients with and without systemic lupus erythematosus (SLE). Although several tests exist for APS diagnosis, their utilization has been highly variable among laboratories and physicians. Therefore, we have evaluated a panel of nine tests and conducted a retrospective study to determine their sensitivity and specificity for supporting the diagnosis of APS in SLE at our Institution between 2010 and 2018.
Methods:
1633 SLE patients, who satisfied the ACR criteria for a definitive diagnosis (Arthritis Rheum. 25, 1271, 1982; Arthritis Rheum. 40, 1725, 1997), were evaluated for the presence of APS as earlier described (J. Thromb. Haemost. 4, 295 (2006). Lupus anticoagulants were assessed by Staclot LA hexagonal phase phospholipid neutralization assay (HPPNA; delta <8 seconds), Staclot diluted Russell viper venom test (dRVVT; <1.2 normalized ratio) obtained from Stago (Parsippany, NJ, USA). Platelet neutralization procedure (PNP; delta < 1 second) has been performed using a STA-R Evolution instrument by Stago, as earlier described (Am. J. Clin. Pathol. 79, 678, 1983; Am. J. Clin. Pathol. 124, 586, 2005). IgG and IgM antibodies against β2-glycoprotein 1 (aβ2-IgG, aβ2-IgM) and cardiolipin (aCL-IgG, aCL-IgM) were measured in house while IgA isotypes (aβ2-IgA, aCL-IgA) were tested by LabCorp Diagnostics (Burlington, NC). Sensitivities, specificities, and positive (PPV) and negative predictive values (NPV) for detection of APS were calculated and compared by 2-tailed chi-square tests using GraphPad software.
Results:
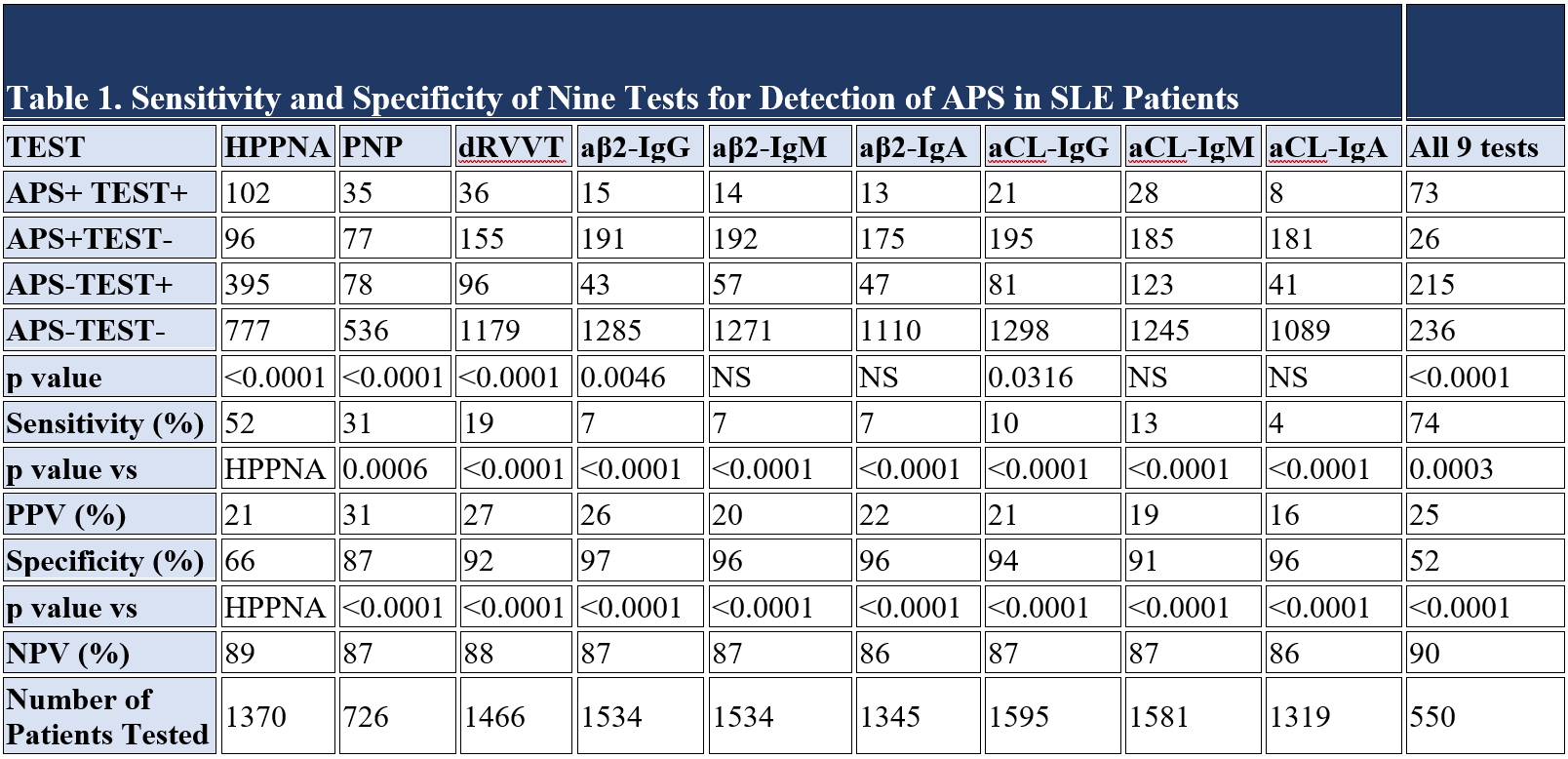
222/1633 SLE patients had APS when using a combination of nine tests. Table 1 shows the frequency of positive and negative test results and p value for each assay. The greatest sensitivity was seen when all nine tests were performed together for detecting APS in SLE patients (74%; χ2 p=0.0003). In contrast, combining all tests had the lowest specificity (52%; p<0.0001). Importantly, the 2nd most sensitive test for detection of APS was the HPPNA at 52%, this tests also had the second lowest specificity (66%). Similar trends were seen when individual APS comorbidities, such as deep venous thrombosis (DVT), pulmonary embolism (PE), and stroke, were separately analyzed. Among the charts reviewed, the complete 9-test panel was only performed in 550 of 1633 patients (Table 1).
Conclusion:
This study demonstrates that utilizing a combined 9-test panel has the greatest sensitivity but lowest specificity for detecting APS in SLE subjects. Thus, a failure to employ the complete panel may lead to exclusion of patients who may meet criteria for identifying patients with APS who need long-term anticoagulation for preventing life-threatening thrombotic events.
To cite this abstract in AMA style:
Sharmeen S, Banki K, Perl A. Combined Panel of Nine Tests Has the Greatest Sensitivity but the Lowest Specificity to Detect Antiphospholipid Antibody Syndrome in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/combined-panel-of-nine-tests-has-the-greatest-sensitivity-but-the-lowest-specificity-to-detect-antiphospholipid-antibody-syndrome-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/combined-panel-of-nine-tests-has-the-greatest-sensitivity-but-the-lowest-specificity-to-detect-antiphospholipid-antibody-syndrome-in-patients-with-systemic-lupus-erythematosus/