Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid Arthritis (RA) is a chronic autoimmune disease with persistent synovial inflammation. Several bDMARDs and tsDMARDs target different key players in the immune-regulatory pathways, including cytokines, JAK, T cells, and B cells. These molecules enable the achievement of remission or LDA in the majority of patients. However, about 20% to 40% of patients fail to achieve remission, and a smaller percentage, recognized as (multi-drug resistance) MDR-RA, fail several bDMARDs and tsDMARDS. In this subset of severe and multi-resistant patients, the combination of a TNFi and a JAKi might be a promising approach, despite not risk-free.
Methods: We performed a descriptive study of patients from the RA UCLouvain Brussels Cohort, who received a combination of TNFi and JAKi. Disease activity trajectory and tolerability, as well as different therapeutic agents received over time, were recorded.
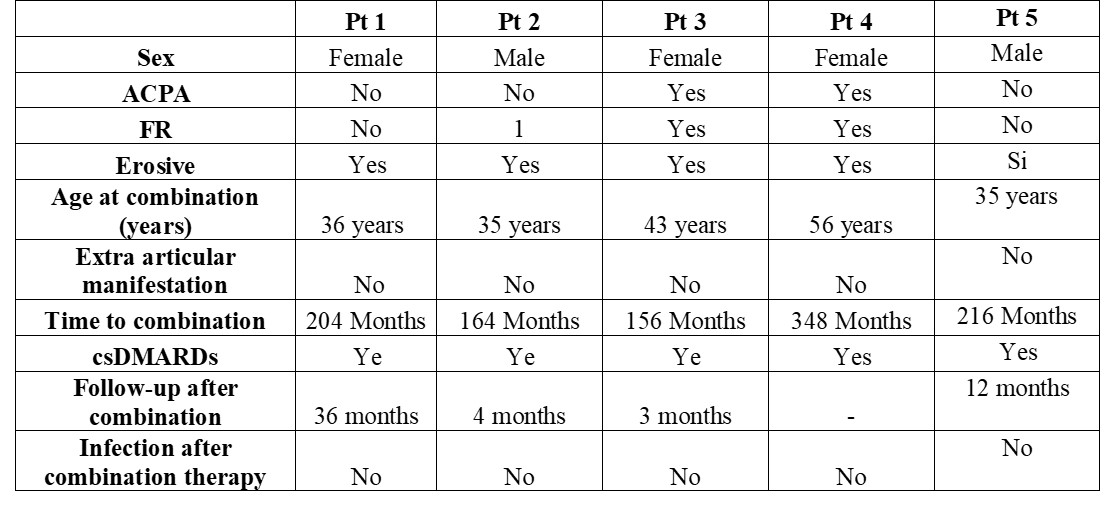
Results: We report five patients (3F, 2M). They received a combination therapy after a median time of 184 months (IQR 116) from diagnosis. The demographic and clinical features for each patient are reported in Table 1. Figure 1 shows disease activity at the moment of each b/tsDMARDs discontinuation (A), reason for discontinuation (B), and the sequence of the b/tsDMARDs (C) for each patient. All of these pts were refractory to 7 bDMARDs and to 2 JAKi. Of note, all the patients received csDMARDs alongside b/tsDMARDs. Variable-dose glucocorticoids have been part of the therapeutic strategy in combination with standard therapy. None of the patients suffered from major adverse events due to b/tsDMARDs as severe infection. All the patients were treated with a TNFi (infliximab or etanercept) associated with a JAKi (Upatacitinib or Filgotinib). Three patients had a minimum follow-up time of 3 months after the combination and then a second evaluation. Pt 1 achieved a persistent remission state up to 3 years of follow-up. We observed a significant decrease in disease activity in two patients, reaching disease remission. None of the patients developed major side effects, including severe infection or hospitalisation, in the observation period.
Conclusion: Our preliminary results indicate that a combination therapy of a TNFi and a JAKi provided good clinical results without safety concerns. In severe and multi-resistant patients, when all classical approach fails to reach a good disease control, the combination therapy could be an option. As infection is the major risk for those patients, a b/tsDMARDs combination should be restricted to young patients with a low infection risk and after adequate vaccinations.
A. Disease activity for each patient according DAS28 disease activity score before starting combination therapy (left) and after initiation of combination therapy (right).
B. Reason for discontinuation for each b/tsDMARDs. From the 5th b/tsDMARDs on, only 3 patients are considered.
C. b/tsDMARDs prescription progression for each patient.
D. Glucocorticoid dosage at each b/tsDMARD change
.jpg) Table 1. Demographic and disease feature for each patient
Table 1. Demographic and disease feature for each patient
To cite this abstract in AMA style:
NATALUCCI F, VAN MULLEM C, AVRAMOVSKA A, SOKOLOVA T, Durez P. Combination Therapy with TNF Inhibitors and JAK Inhibitors in Multi-Drug-Resistant Rheumatoid Arthritis: A Case Series from the RA UCLouvain Brussels Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/combination-therapy-with-tnf-inhibitors-and-jak-inhibitors-in-multi-drug-resistant-rheumatoid-arthritis-a-case-series-from-the-ra-uclouvain-brussels-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/combination-therapy-with-tnf-inhibitors-and-jak-inhibitors-in-multi-drug-resistant-rheumatoid-arthritis-a-case-series-from-the-ra-uclouvain-brussels-cohort/