Session Information
Session Type: Abstract Session
Session Time: 12:00PM-12:50PM
Background/Purpose: Increased electronic health record (EHR) administrative workload is a great source of physician dissatisfaction. We embedded pharmacists into our Rheumatology team in 2019. This study explored the impact of pharmacist integration on reducing physician workload and burnout.
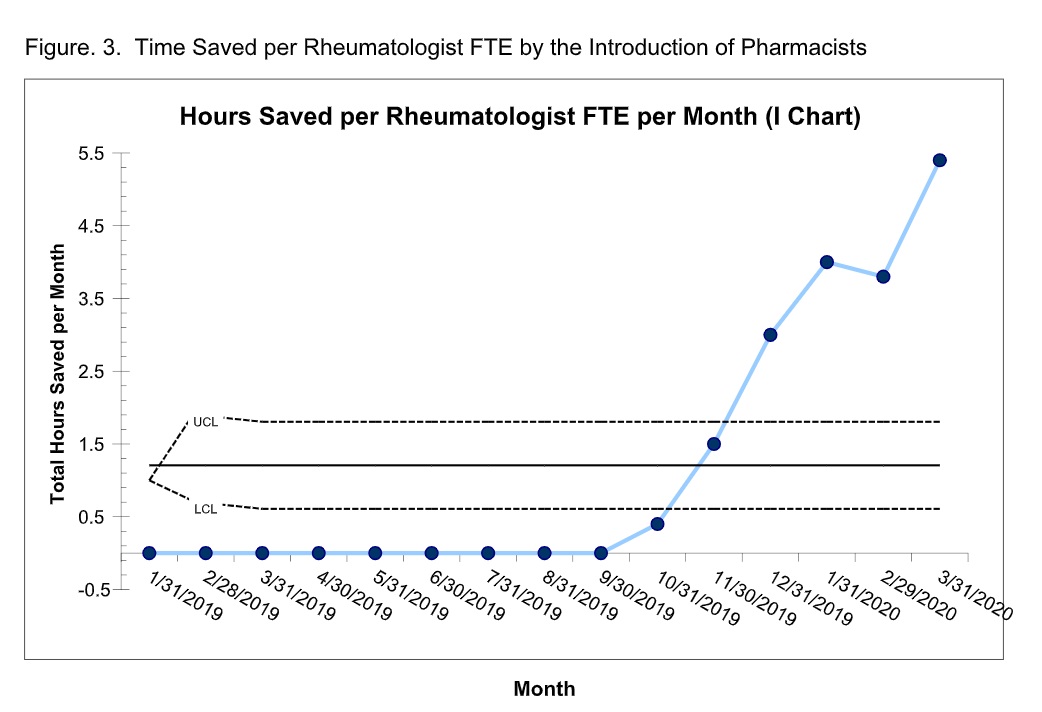
Methods: The monthly volume of medication refills by rheumatologists was measured as a baseline from 1/30/2019 to 9/30/2019 within our EHR (Epic). Protocol driven medication refill parameters for DMARDs and non-DMARDs were created per American College of Rheumatology guidelines. Using these refill parameters, physician time needed per refill was derived by averaging the time per message for 40 refills across 5 physicians. After implementation of pharmacists, the monthly volume of refills by pharmacists and physicians was measured from 10/1/2019 to 3/31/2020. Total physician time saved was calculated by multiplying the number of pharmacist refill encounters with average physician refill time. The time saved per month was divided by the number of clinical full-time equivalents to calculate the time saved per rheumatologist. Shewhart P-charts were used to measure significance for volume and time saved. Rheumatologists’ satisfaction with EHR work was gauged via anonymous electronic survey pre- and post-pharmacist addition. Satisfaction was rated from 1 (not happy) to 5 (high satisfaction). Two additional questions were asked in the post pharmacist survey related to effect on work and burnout. 100% of physicians responded to the pre-survey and 93% of physicians responded to the post survey.
Results: The volume of medication refills by physicians decreased from about 1201 refills per month (or 100% of all refills) pre-pharmacist to 464 refills per month (or 27% of all refills) post-pharmacist integration (Figure1). The total time saved for all the rheumatologists (15 physicians, 7.75 FTEs) increased from 0 hours per month pre-pharmacist in September 2019 to 41.5 hours per month post-pharmacist in March 2020 (Fig.2). The time saved per physician FTE increased from 0 hours per month in September 2019 to 5.4 hours per month in March 2020 (Fig.3). Shewhart P chart analysis met statistical significance for time saved per the individual and group of rheumatologists respectively with the implementation of pharmacists in our team. The surveys showed that the mean satisfaction with EHR refill work improved from 1.4 +/-0.2 at baseline to 4.3 +/-0.2 (p< 0.001) post pharmacist introduction. 100% of physicians reported that the pharmacist addition to their daily workflow helped them leave work on time and their workload interfered less with life outside of work (n=14), and 79% of physicians reported less burn out.
Conclusion: In early 2020, 51% of rheumatologists reported burnout in the workplace. This negatively impacts physician work effort, patient outcomes, and healthcare costs. Our study showed that pharmacists’ medication refills alone have decreased physician EHR work and burnout. This shows great potential for other areas of improvement through pharmacist integration. Implementing a pharmacist into practice has brought us closer to achieving the 4th Aim of Quadruple Aim-improving the work life of the rheumatologist.
To cite this abstract in AMA style:
Rottmann E, Cote J, Thomas S, Grassi D, Chronowski J, Schroeder L, Pugliese D, Newman E. Combating Rheumatologist Burnout: Use of Protocol Driven Medication Refill by Pharmacists [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/combating-rheumatologist-burnout-use-of-protocol-driven-medication-refill-by-pharmacists/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/combating-rheumatologist-burnout-use-of-protocol-driven-medication-refill-by-pharmacists/