Session Information
Session Type: ACR Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Giant cell arteritis (GCA) is a clinically heterogeneous disease. Disease subsets based upon cranial versus extracranial artery involvement have been proposed. The study objective was to determine if GCA subsets are associated with distinct clinical profiles or merely reflective of differential diagnostic assessment.
Methods: Patients were included from a large international cohort with standardized data collection. Patients with a confirmed diagnosis of GCA were divided into four subsets based on a temporal artery (TA) abnormality [definite vasculitis by biopsy (TAB) or halo-sign positive ultrasound (TA-US)] and/or imaging evidence of large-vessel (LV, aorta and/or its primary branches) involvement on imaging: 1) patients with evidence of both LV involvement and TA abnormality (TA(+)/LV(+) GCA); 2) patients with TA abnormality without LV involvement (TA(+)/LV(-) GCA); 3) patients with LV involvement without TA abnormality (TA(-)/LV(+) GCA); and 4) patients with a clinical diagnosis of GCA without LV involvement or TA abnormality (TA(-)/LV(-) GCA).
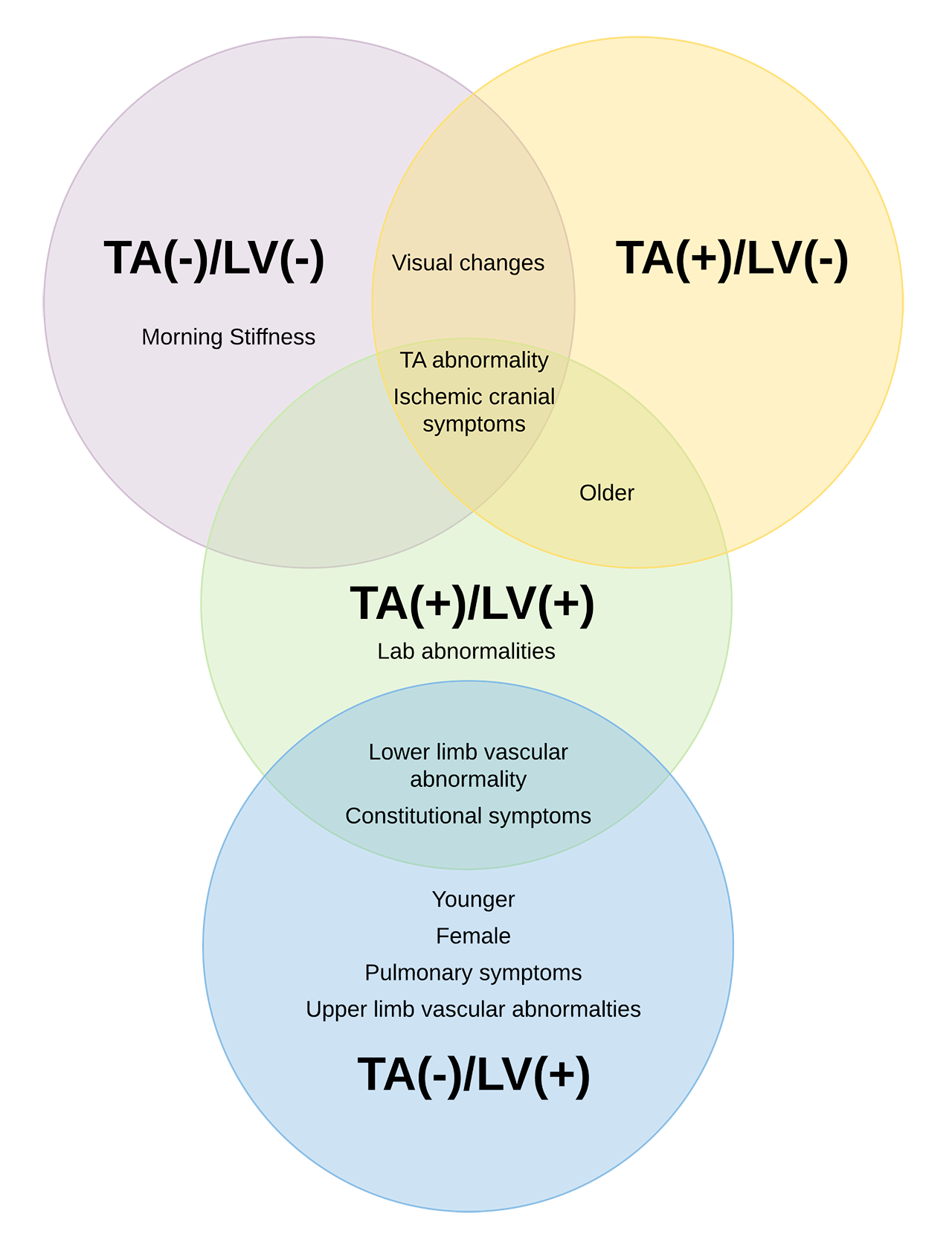
Results: Out of 941 patients, 329 (35%) had TA-US, 705 (75%) had TAB, 536 (57%) had LV imaging, and 431 (46%) had both LV imaging and TA-US/TAB. GCA subsets had distinct clinical profiles (Figure). TA(+)/LV(-) GCA (n=480) had the highest burden of visual changes (e.g. amaurosis fugax, sudden ongoing visual loss; p< 0.01), other cranial ischemic symptoms (e.g. jaw claudication, scalp tenderness; p< 0.01), and TA abnormalities on physical examination (p< 0.01), with little evidence of other vascular exam abnormalities. Patients with TA(-)/LV(-) GCA (n= 245) were nearly indistinguishable from TA(+)/LV(-) GCA with a high prevalence of visual changes and other cranial ischemic symptoms (p< 0.01) but also had a high burden of musculoskeletal symptoms (p=0.02). Patients with TA(-)/LV(+) GCA (n=116) were younger (p< 0.01) and more frequently female (p< 0.01), with a lower burden of visual changes (p< 0.01) and cranial ischemic symptoms (p< 0.01), and a higher burden of vascular abnormalities (e.g. upper/lower limb claudication/pulse abnormality, arterial bruit, blood pressure differences; p< 0.01), constitutional (e.g. weight loss, night sweats; p< 0.01), and pulmonary symptoms (e.g. non-productive cough, dyspnea; p< 0.01). Patients with TA(+)/LV(+) GCA (n=100) were older and more likely to be male with a high prevalence of cranial ischemic symptoms like TA(+)/LV(-) GCA and a high prevalence of lower-limb vascular abnormalities and constitutional symptoms like TA(-)/LV(+) GCA. Patients with TA(+)/LV(+) GCA also had the highest prevalence of lab abnormalities (p< 0.01). When analyses were restricted to 431 patients who had both TA assessment (TAB or TA-US) and LV assessment by imaging, the four subsets had similar patterns of clinical associations.
Conclusion: Patients with GCA can be divided into subsets based on temporal and extracranial artery involvement. Each subset has a unique clinical profile that is not explained by differences in diagnostic assessment. Longitudinal studies comparing immunologic differences and clinical outcomes across these subsets are warranted.
To cite this abstract in AMA style:
Gribbons K, Ponte C, Craven A, Robson J, Suppiah R, Watts R, Luqmani R, Merkel P, Grayson P. Clinical Subsets in Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/clinical-subsets-in-giant-cell-arteritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-subsets-in-giant-cell-arteritis/