Session Information
Date: Sunday, October 26, 2025
Session Type: Abstract Session
Session Time: 1:15PM-1:30PM
Background/Purpose: Still’s disease (SD) is a autoinflammatory disease (AID) characterized by a wide range of clinical manifestations and can exhibit life-threatening macrophage activation syndrome (MAS). Procalcitonin (PCT), a potential biomarker in SD, may be increased even in the absence of infection. The nature of PCT in AIDs remains unclear. We aimed to reveal the relationship between non-infectious increased PCT and the clinical features of SD.
Methods: In this retrospective study, patients with available PCT data at the time of diagnosis and fulfilling the Yamaguchi criteria were enrolled, as well as age- and sex-matched healthy individuals. Patients with any suspicious or documented infection at the time of diagnosis and/or during the active disease course and other factors that increase PCT, such as impaired renal function, were excluded from the study. Patients were classified into two groups based on the cut-off value of PCT, which was 0.5 ng/dl. Findings during the active disease, treatment, and laboratory parameters were evaluated.
Results: This study was conducted with 110 patients. PCT levels in SD, SD without MAS, and SD with MAS were significantly higher compared with healthy control (0.04 [0.03-0.04] ng/ml) (all three p< 0.001). PCT levels in SD with MAS were also significantly higher than SD without MAS (p=0.002) (Figure 1). Seventy-five (68%) patients were in the PCT < 0.5 group, and 35 (32%) patients were in the PCT ≥0.5 group. Patients’ characteristics are shown in Table 1. Pleuritis and MAS were more frequent in the PCT ≥0.5 group (p=0.004, p=0.001, respectively). mPouchet score was significantly higher in the PCT ≥0.5 group (p=0.017). The requirement for bDMARD, especially anakinra, was higher in the PCT ≥0.5 group (p=0.051, p=0.008, respectively). Laboratory parameters of the patients are presented in Table 2. Platelet count was lower; thus, thrombocytopenia was higher in the PCT ≥0.5 group (p=0.008, p=0.011, respectively). AST and LDH levels were significantly higher in the PCT ≥0.5 group (p=0.006, p< 0.001, respectively). CRP and ferritin levels were significantly higher in the PCT ≥0.5 group, whereas albumin was lower (p=0.013, p< 0.001, and p=0.002, respectively). There was a positive correlation between PCT levels and AST, LDH, CRP, and ferritin levels (r=0.339, p< 0.001; r=0.584, p< 0.001; r=0.288, p< 0.01; and r=0.499, p< 0.001, respectively). In univariate logistic regression analysis, the risk for development of MAS was up to 6.4-fold in the PCT ≥0.5 group (crude OR 6.4 [CI 95% 2.0-20.4], p=0.002), while up to 4.3-fold in multivariate logistic regression analysis (adjusted OR 4.3 [CI 95% 1.1-16.8], p=0.038). Normalization of PCT levels occurred in all patients after immunosuppressive treatment.
Conclusion: According to the results of this preliminary study, the high risk of developing MAS and the requirement of bDMARD are indicative of a high inflammatory response in patients with increased PCT. Our results provide evidence that high PCT in SD is a potential independent predictor of MAS. PCT may be a convincible marker in AIDs like other well-known inflammatory parameters. Further studies are warranted to confirm the study findings in larger cohorts and to explain the mechanism of PCT elevation in AIDs.
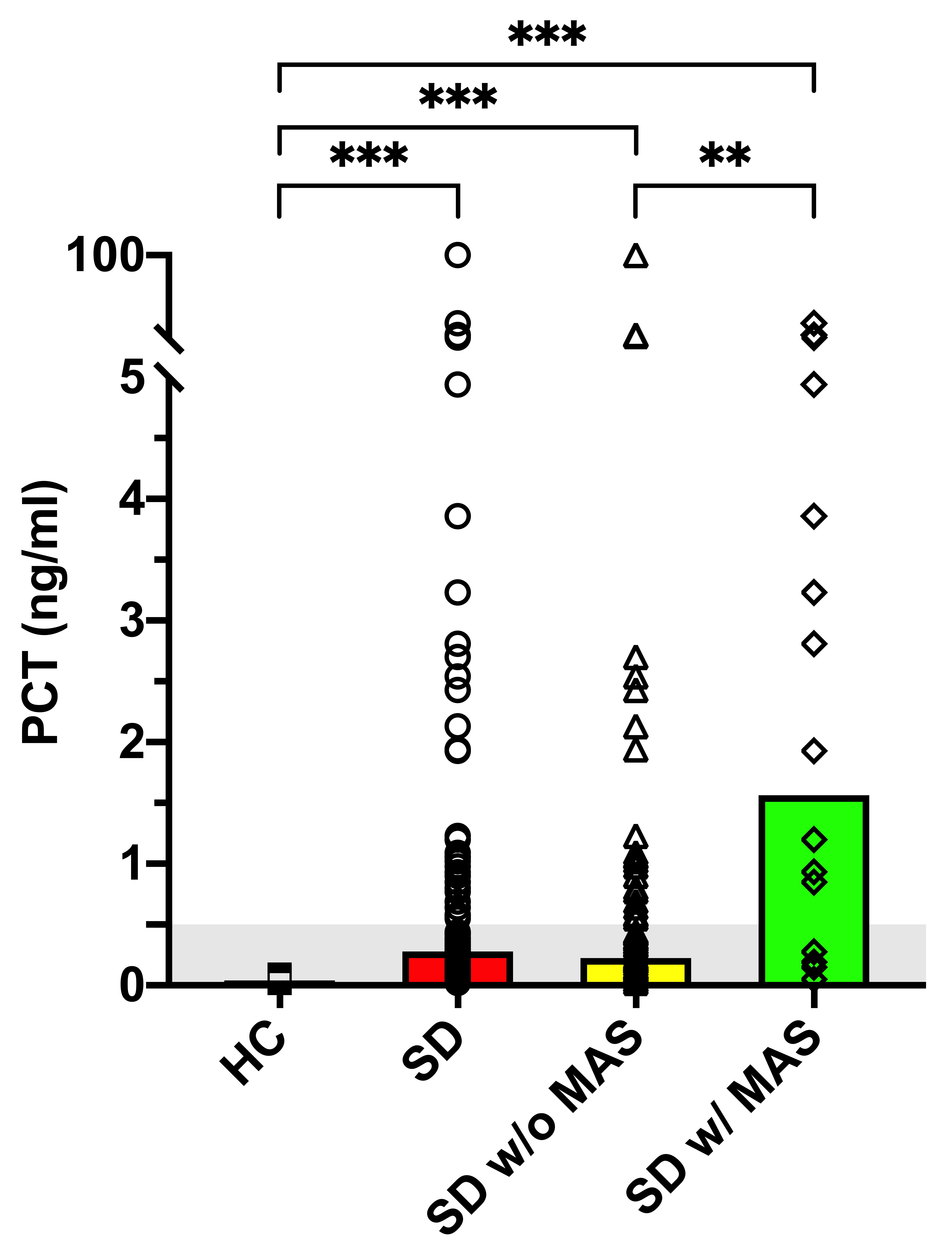 Figure 1. Procalcitonin (PCT) levels of patients with Still’s disease (SD) (n=110), SD without macrophage activation syndrome (MAS) (n=94), and SD with MAS (n=16) at the time of diagnosis and healthy control (HC) (n=50). Bars show the median value. Mann-Whitney U; ** p < 0.01, *** p < 0.001.
Figure 1. Procalcitonin (PCT) levels of patients with Still’s disease (SD) (n=110), SD without macrophage activation syndrome (MAS) (n=94), and SD with MAS (n=16) at the time of diagnosis and healthy control (HC) (n=50). Bars show the median value. Mann-Whitney U; ** p < 0.01, *** p < 0.001.
.jpg) †Fisher’s Exact, ‡Chi-Square, and ¢Mann-Whitney U. Abbreviations: bDMARD, biologic disease modifying anti-rheumatic drug; csDMARD, conventional synthetic disease modifying anti-rheumatic drug; DAH, diffuse alveolar hemorrhage; DIC, disseminated intravascular coagulation; IQR, interquartile range; IVIG, intravenous immunoglobulin; m, months; MAS, macrophage activation syndrome; med, median; MPRD, methylprednisolone; n, number of patients; y, years.
†Fisher’s Exact, ‡Chi-Square, and ¢Mann-Whitney U. Abbreviations: bDMARD, biologic disease modifying anti-rheumatic drug; csDMARD, conventional synthetic disease modifying anti-rheumatic drug; DAH, diffuse alveolar hemorrhage; DIC, disseminated intravascular coagulation; IQR, interquartile range; IVIG, intravenous immunoglobulin; m, months; MAS, macrophage activation syndrome; med, median; MPRD, methylprednisolone; n, number of patients; y, years.
.jpg) †Fisher’s Exact, ‡Chi-Square, ¢Mann-Whitney U, and ¥Student’s-t test. Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, c-reactive protein; ESR, erythrocyte sedimentation rate; IQR, interquartile range; LDH, lactate dehydrogenase; LFT, liver function tests; med, median; n, number of patients; PCT, procalcitonin; PMNL, polymorphonuclear leukocytes; SD, standard deviation; ULN, upper limit of normal; WBC, white blood cell.
†Fisher’s Exact, ‡Chi-Square, ¢Mann-Whitney U, and ¥Student’s-t test. Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, c-reactive protein; ESR, erythrocyte sedimentation rate; IQR, interquartile range; LDH, lactate dehydrogenase; LFT, liver function tests; med, median; n, number of patients; PCT, procalcitonin; PMNL, polymorphonuclear leukocytes; SD, standard deviation; ULN, upper limit of normal; WBC, white blood cell.
To cite this abstract in AMA style:
Bektas E, Uludogan B, Fırlatan Yazgan B, Kilinc O, Acar B, Kizilkaya O, Yilmaz A, Yuce B, Ugurlu s, Kalyoncu U, Kasifoglu T, Bes C. Clinical significance of non-infectious increased procalcitonin in Still’s disease: A predictor of macrophage activation syndrome [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-significance-of-non-infectious-increased-procalcitonin-in-stills-disease-a-predictor-of-macrophage-activation-syndrome/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-significance-of-non-infectious-increased-procalcitonin-in-stills-disease-a-predictor-of-macrophage-activation-syndrome/
