Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Prosthetic joint septic arthritis (PJSA) complicates about 1 to 2 percent of joint replacement surgeries. The management of PJSA usually includes a combination of surgery and antibiotics. Resection arthroplasty with re-implantation for PJSA may be performed in one or two stages. There is a lack of comparative trials comparing the two strategies and there is no consensus regarding which option should be recommended.
Objective: To define the epidemiology, clinical characteristics and outcomes of patients with PJSA for whom a one-stage procedure was performed as compared with patients with PJSA for whom a two-stage procedure was performed.
Methods: We conducted a retrospective study that included all patients aged 18 years and older admitted to a single, tertiary-care hospital between 1998 and 2015 who were diagnosed with monoarticular PJSA and were surgically treated with either a one-stage or two-stage joint replacement. We excluded cases of native joint infection or septic bursitis.
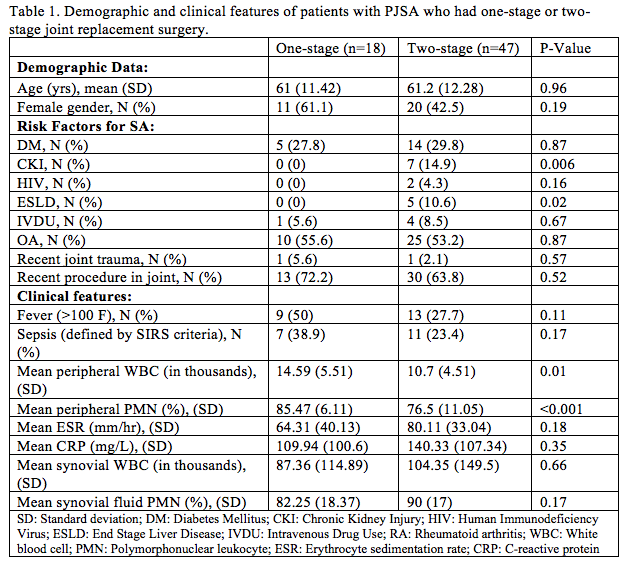
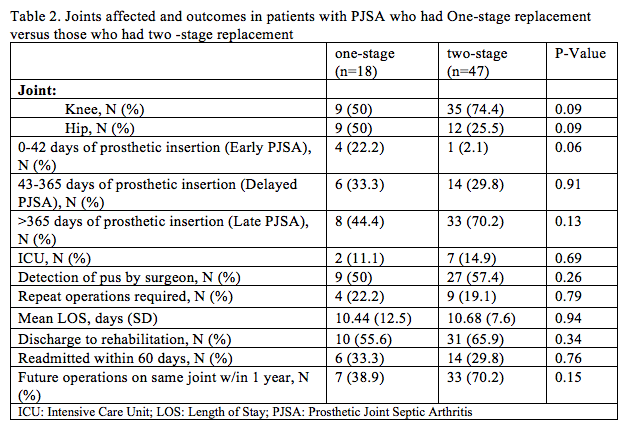
Results: Of the 65 patients with PJSA treated with either one- or two-stage procedure, 18 had a one-stage procedure while 47 had a two-stage procedure. There were no differences in average age or gender between the two groups [Table 1]. Chronic kidney injury and end-stage liver disease were significantly more common in patients who had a two-stage procedure (p=0.006 and p=0.02 respectively) while patients who had a one-stage replacement were more often febrile (50% vs. 27.7%; p=0.11), had higher peripheral white blood cell (WBC) counts (14.6 vs. 10.7 thousand cells/mm3; p=0.01) and had a greater mean percentage of peripheral polymorphonuclear (PMN) leukocytes (85.5% vs. 76.5%, p<0.001). While one-stage procedures were split evenly between knee and hip replacements, two-stage knee replacements were more common (75% of cases) than two-stage hip replacements (25% of cases) [Table 2]. Outcomes between the two strategies were similar [Table 2].
Conclusion: In our institution, two-stage joint revision for PJSA is more common than one-stage procedures, especially when the knee is involved. Although this study might have been underpowered to detect small differences, there were no clear differences in clinical features or outcomes of patients with PJSA undergoing revision arthroplasty based on the type of operation. Surgeons seem to favor two-stage for patients with comorbidities while preferring one-stage for patients presenting with early PJSA infection. Larger prospective trials are needed to identify which circumstances should lead surgeons to choose one strategy over the other.
To cite this abstract in AMA style:
Fowler ML, Byrne K, Lieber S, Shmerling R, Paz Z. Clinical Presentation and Outcomes in Patients with Prosthetic Joint Septic Arthritis Who Had One-Stage Versus Two-Stage Joint Replacement [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/clinical-presentation-and-outcomes-in-patients-with-prosthetic-joint-septic-arthritis-who-had-one-stage-versus-two-stage-joint-replacement/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-presentation-and-outcomes-in-patients-with-prosthetic-joint-septic-arthritis-who-had-one-stage-versus-two-stage-joint-replacement/