Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Prescription opioids for non-cancer pain in the UK have increased considerably over the past two decades, alongside a rise in associated harms. Despite the high prevalence of opioid use, there are limited data on the specific indications for prescribing opioids for non-cancer pain. By understanding the reasons for opioid initiation and relative contribution of systems and specific conditions, the opioid burden in patient subgroups can be assessed to develop tailored interventions, policies, and additional support as appropriate. The aim was to evaluate indications associated with new opioid initiation in non-cancer pain using nationally representative UK data.
Methods: Data from the Clinical Practice Research Datalink (CPRD) AURUM were used, a nationally representative database of anonymised electronic health records from General Practices across the UK, between 1/1/06 to 31/09/21. People ≥18 years who were new users of opioids were included. Exclusion criteria included a cancer diagnosis five years prior to first opioid prescription (index date) and methadone users. SNOMED-CT code lists were derived for conditions associated with opioid use following consultation with GPs, rheumatologists, pharmacists, and chronic pain specialists. These were applied to a period one-year prior to index date for surgical indication and five years prior for chronic conditions. Descriptive statistics were used to analyse the data using STATA v13.1, allowing for overlap between indications.
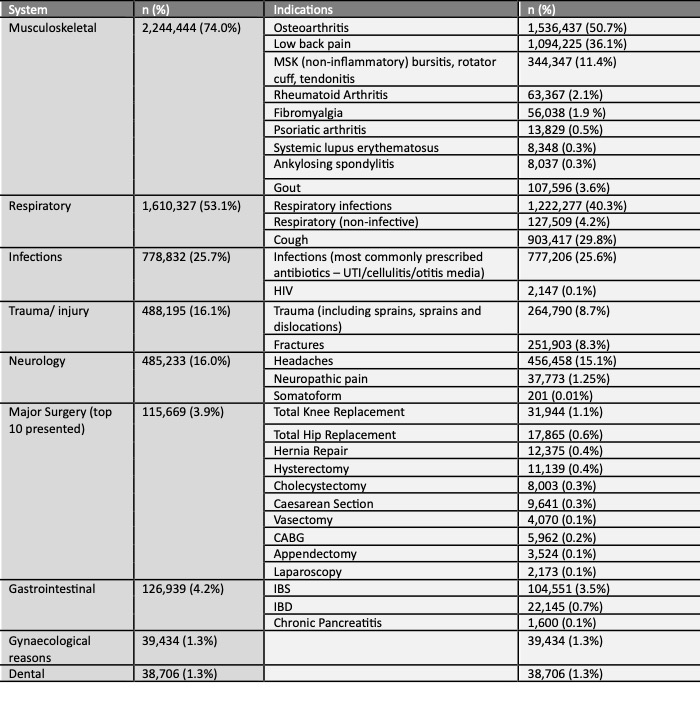
Results: A total of 3,032,185 patients classed as new opioid users over the ~15-year study window were identified. Opioids were initiated more commonly in women (60.7%), people aged 45-64 (40.0%) and ≥65 years (37.0%). We identified 9 systems associated with initiating opioids. The most common were musculoskeletal (73.2%), respiratory (53.1%), infections (25.7%), trauma/injury (16.1%), neurology (16.0%), gastrointestinal (4.2%) and post-surgical (3.9%) (Table 1). Musculoskeletal (MSK) conditions that were most frequently associated with opioid use were osteoarthritis (n=1,536,437, 50.7%), low back pain (1,094,225, 36.1%), other non-inflammatory MSK conditions (e.g. rotator cuff tears), rheumatoid arthritis (63,367, 2.2%) and fibromyalgia (56,038, 1.9%). Post-surgical indications one year prior to index date were associated with 3.9% of all prescriptions. Orthopaedic surgeries were the most common and contributed to 42.1% all post-surgical indications (Table 1). This included total knee replacements (n= 31,944; 27.6%) and total hip replacements (n=17,865; 14.5%) of all post-surgical indications.
Conclusion: This is the first study in the UK evaluating large scale national data to assess indications associated with opioid initiation. Almost three quarters of the new prescriptions of opioids for non-cancer pain were in people with a diagnosis of a MSK condition. Orthopaedic surgeries contributed to a third of all post-surgical indications. These findings could help prioritise efforts for targeted interventions in opioid prescribing, clinical vigilance and future policy to support non-pharmacological interventions.
To cite this abstract in AMA style:
Lyon M, Ramirez Medina C, Davies E, Jani M. Clinical Indications Associated with New Opioid Use for Pain Management in the United Kingdom Using National Primary Care Data [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/clinical-indications-associated-with-new-opioid-use-for-pain-management-in-the-united-kingdom-using-national-primary-care-data/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-indications-associated-with-new-opioid-use-for-pain-management-in-the-united-kingdom-using-national-primary-care-data/