Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: We aimed to investigate the relationship between hydralazine and any form of vasculitis (small, medium, or large vessel), to describe clinical features and outcomes of patients with hydralazine-associated vasculitis, and to compare them to a case control cohort of primary vasculitis.
Methods: We performed a retrospective study. First, patients who had been diagnosed with ANCA-associated vasculitis (AAV) at Mayo Clinic between 1996 and 2022 were reviewed for hydralazine usage. Second, we searched the electronic medical record for all patients who were prescribed hydralazine and matched the following key terms: vasculitis renal, vasculitis pulmonary, vasculitis urticarial, vasculitis hypersensitivity, vasculitis necrotizing, vasculitis leukoclastic, vasculitis cutaneous, vasculitis personal history, arteritis giant cell, giant cell arteritis personal history, giant cell arteritis with polymyalgia rheumatica, aortic arch syndrome ,Takayasu, arteritis Takayasu, polyarteritis nodosa, polyarteritis nodosa microscopic, other conditions related to polyarteritis nodosa. In addition, we queried the patients who had been prescribed hydralazine for positive ANCA test results. We then matched each patient diagnosed with hydralazine-associated vasculitis and primary vasculitis with two controls by gender, age at diagnosis and dominant ANCA-type.
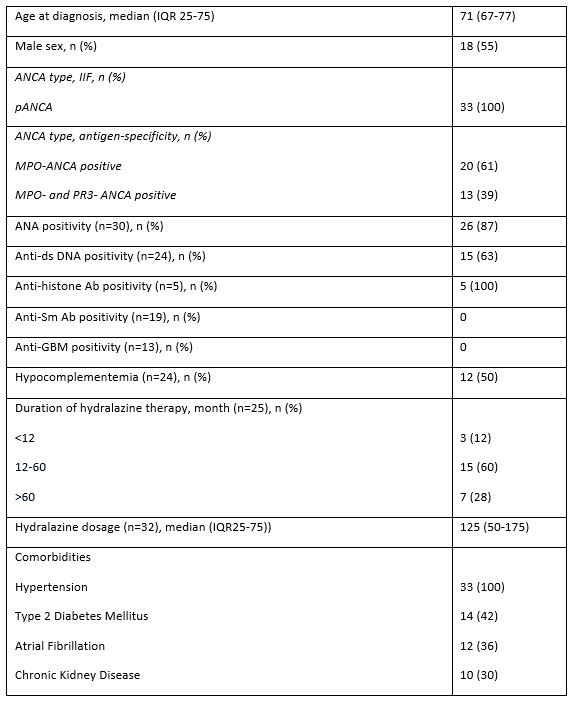
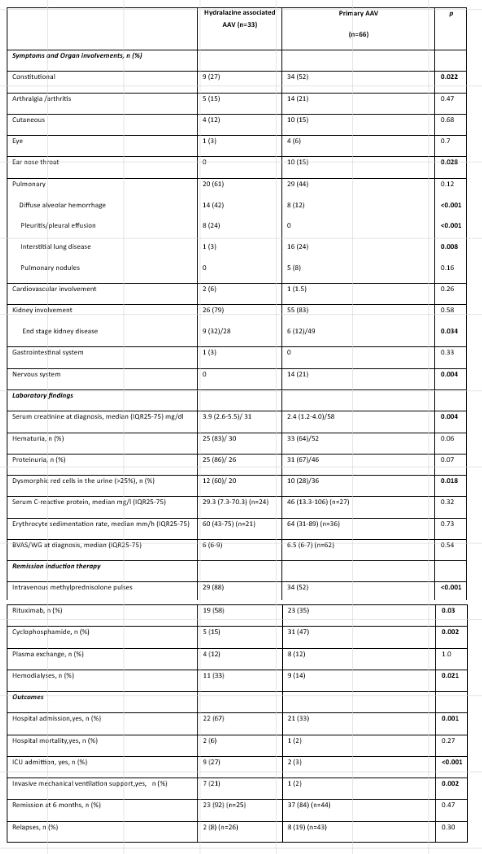
Results: We found that hydralazine was associated only with AAV and not with other forms of vasculitis. Thirty-three patients (55% male; median age [IQR] at diagnosis 71[67-77]) with hydralazine-associated AAV were included. All 33 patients were p-ANCA positive. Twenty patients (61%) had MPO-ANCA, and 13 patients (39%) had both MPO- and PR3-ANCA (MPO-ANCA titers being consistently higher than PR3-ANCA titers). Glomerulonephritis (79%) and pulmonary manifestations were most common (61%) (Table 1). Diffuse alveolar hemorrhage (42% vs 12%; p< 0.001) and pleuritis (24% vs 0, p< 0.001) were more common among patients with hydralazine-associated AAV compared to 66 matched patients with primary AAV, whereas constitutional symptoms (27% vs 52%, p=0.02), interstitial lung disease (3% vs 24%, p=0.008), ear nose throat ( 0 vs 15%, p=0.03) and nervous system involvement (0 vs 21%, p=0.004) were more common in primary AAV. Moreover, remission at 6 months was achieved more frequently in patients with hydralazine-associated AAV (p< 0.001) (Table 2).
Conclusion: Hydralazine was only associated with AAV and not with other forms of vasculitis. Hydralazine-associated AAV resembles microscopic polyangiitis, and MPO-ANCA is the predominant ANCA-type. In contrast to primary AAV, hydralazine-associated AAV seems to have organ predilection for kidneys and lungs. Prompt diagnosis and treatment is crucial as discontinuation of hydralazine and immunosuppressive therapy can improve outcomes.
To cite this abstract in AMA style:
Ediboglu E, Falde S, Baqir M, Cartin-Ceba R, Specks U. Clinical Features and Outcomes of Hydralazine-associated Vasculitis: A Case-Control Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-features-and-outcomes-of-hydralazine-associated-vasculitis-a-case-control-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-and-outcomes-of-hydralazine-associated-vasculitis-a-case-control-study/