Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory
ocular disease (IOD) has traditionally been regarded as a severe
extra-articular manifestation of rheumatoid arthritis (RA) with high mortality.
This study aims to evaluate episcleritis (EP) and scleritis (SC) among a recent
large single-institution cohort of patients with RA to determine clinical correlates,
outcomes and risk factors.
Methods:
A retrospective review was performed to assemble a cohort of patients with EP
and SC among RA patients evaluated between 1/1/1996-12/31/2013. All cases met
the 1987 ACR criteria for RA. Cases were compared to age- and sex-matched comparators
with RA without IOD to identify risk factors. Chi-square and rank sum tests
were used to compare characteristics between groups. Kaplan-Meier methods were
used to analyze outcomes.
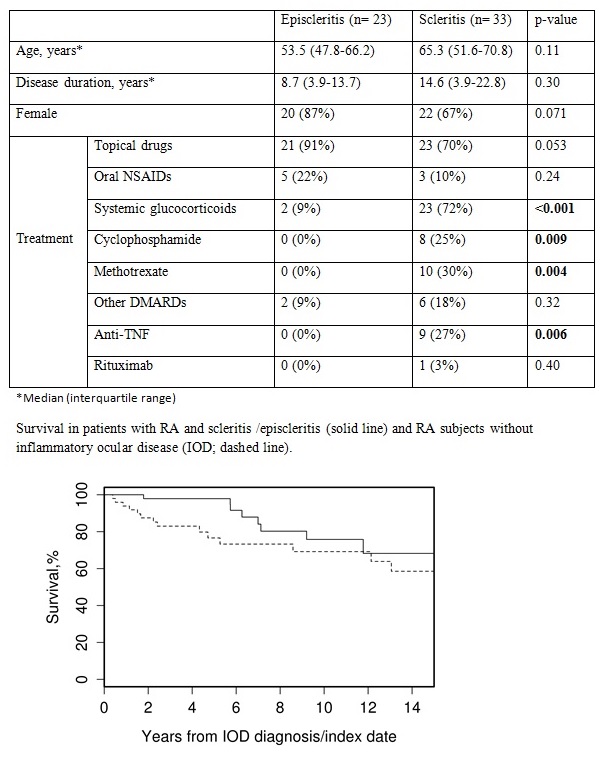
Results: We
identified 56 patients (75% female, 92% white, mean age 60 y) with IOD (23 EP,
33 SC). Median follow up was 6.6 y (IQR 4.6 – 13.1) for EP and 3.1 y (IQR
1.3-5.9) for SC. One third had bilateral eye involvement (74 eyes). Majority
had seropositive, erosive RA with a median duration of 10.8 y (IQR 3.9-22.2). Although
clinical presentation was similar, with conjunctival injection noted in
majority, eye pain and headache were more common with SC. Markers of
inflammation were elevated in 7/15 SC and 6/15 EP.
EP was primarily
treated with topical therapy but SC required systemic therapy (Table) and
immunosuppressive agents. SC patients experienced greater loss of visual acuity
during disease course (mean 0.3 vs 0.1 logMAR, p = 0.002). At 1 year, the cumulative
incidence (CI) of resolution was 65% for EP vs 30% for SC (HR 0.61, p = 0.11)
and CI of a new episode of IOD was 10% for EP vs 31% for SC (HR 2.71, p=0.14).
The 56 patients with IOD
were compared to 54 age, sex and disease duration matched subjects with RA but
without IOD (median disease duration 10.8 y vs. 9.9 y, p = 0.54; median follow
up 5.9 y (IQR 2.7-10.4) for IOD patients and 4.3 y (IQR 1.7-10.9) for comparators).
Cases had a higher prevalence of severe extra-articular manifestation (ExRA)
(Malmo criteria) (25% vs 4%, p = 0.002) and dry eye syndrome (43% vs 19%, p =
0.007). Ten year survival was 76% for IOD vs 69% for non-IOD subjects (HR 0.49:
95% CI: 0.21-1.16, p = 0.10). Patients with SC had a somewhat higher mortality
than EP (HR 3.96, 95%CI 0.79-19.75, p=0.094). The incidence of cardiovascular
events in 5-years follow up was similar among cases and non-IOD subjects (13%
vs 12%, p = 0.933), while new ExRA were more frequent in cases (41% vs 8%, p =
0.006).
Conclusion: Severe
ExRA and dry eye syndrome are associated with increased risk of developing SC
and EP in patients with RA. SC and EP further predispose to developing
additional ExRA, increasing the burden of disease. In contrast to older
literature, survival among IOD patients is now at least as good as in those
without IOD, perhaps due to modern RA treatment strategies or secular disease
trends.
To cite this abstract in AMA style:
Caimmi C, Smith WM, Crowson CS, Matteson EL, Makol A. Clinical Correlates, Outcomes and Predictors of Episcleritis and Scleritis Associated with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/clinical-correlates-outcomes-and-predictors-of-episcleritis-and-scleritis-associated-with-rheumatoid-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-correlates-outcomes-and-predictors-of-episcleritis-and-scleritis-associated-with-rheumatoid-arthritis/