Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: In recent years, the number of older patients with systemic lupus erythematosus (SLE) in Japan has been increasing, with particular attention to those developing SLE over the age of 70. This study investigates the clinical characteristics, gender differences, treatment response, and prognosis of late-onset SLE patients compared with young-onset SLE patients.
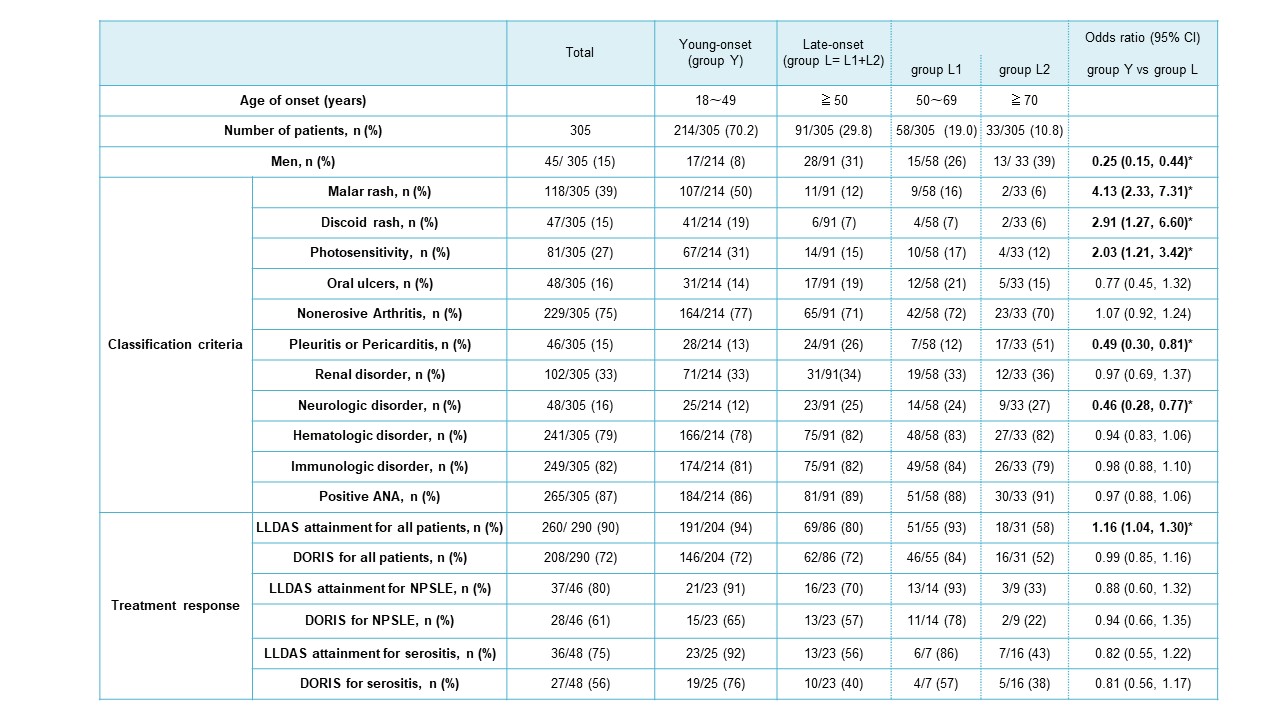
Methods: This retrospective study included 305 SLE patients attending Tohoku Medical Pharmaceutical University Hospital between 1984 and 2023, comprising 45 men and 260 women. They were divided into three groups based on their age at diagnosis of SLE according to the 1997 classification criteria: young-onset patients between 8 and 49 years of age (group Y), late-onset patients aged 50 years or older (group L). Group L was further divided into two subgroups: onset between 50 and 69 years of age (group L1) and onset at 70 years or older (group L2). The Y, L1, and L2 groups consisted of 214, 58, and 33 cases, respectively, of which 17, 15, and 13 were men. We compared organ lesions by groups and analyzed relative risk ratios for differences according to age groups. Lupus low disease activity state (LLDAS) attainment and a definition of remission in SLE (DORIS) were also assessed in each age group.
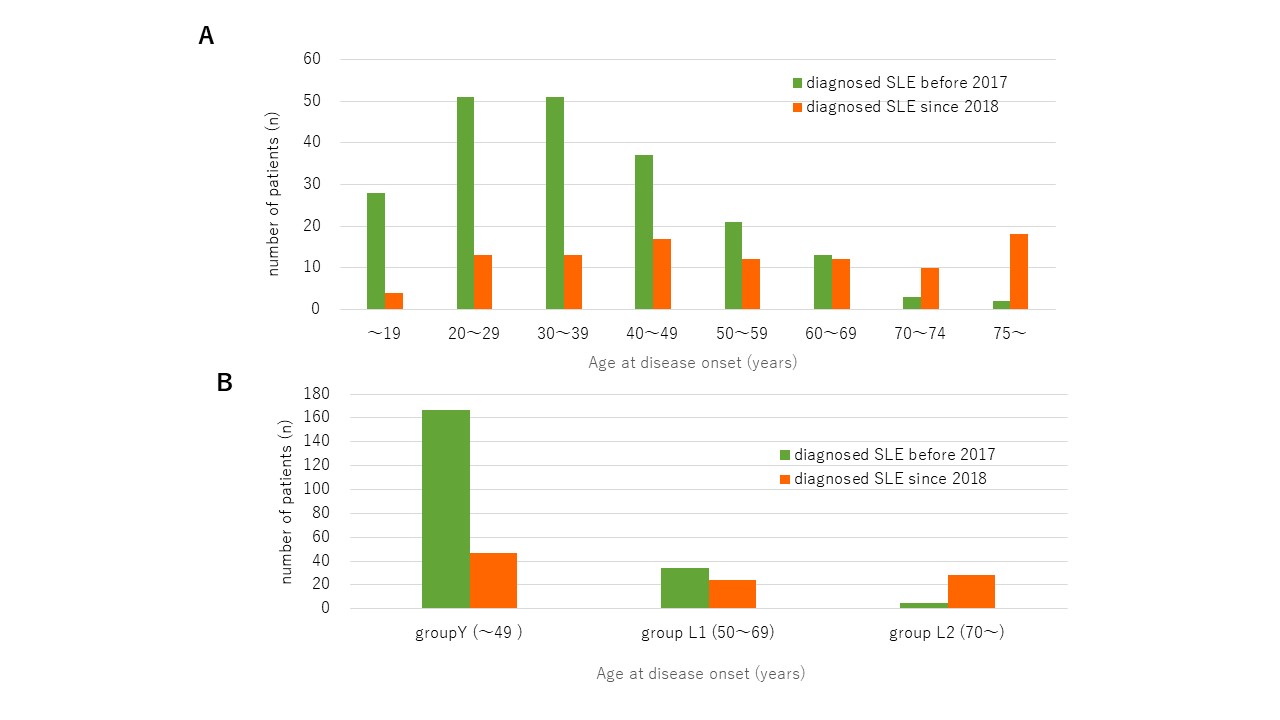
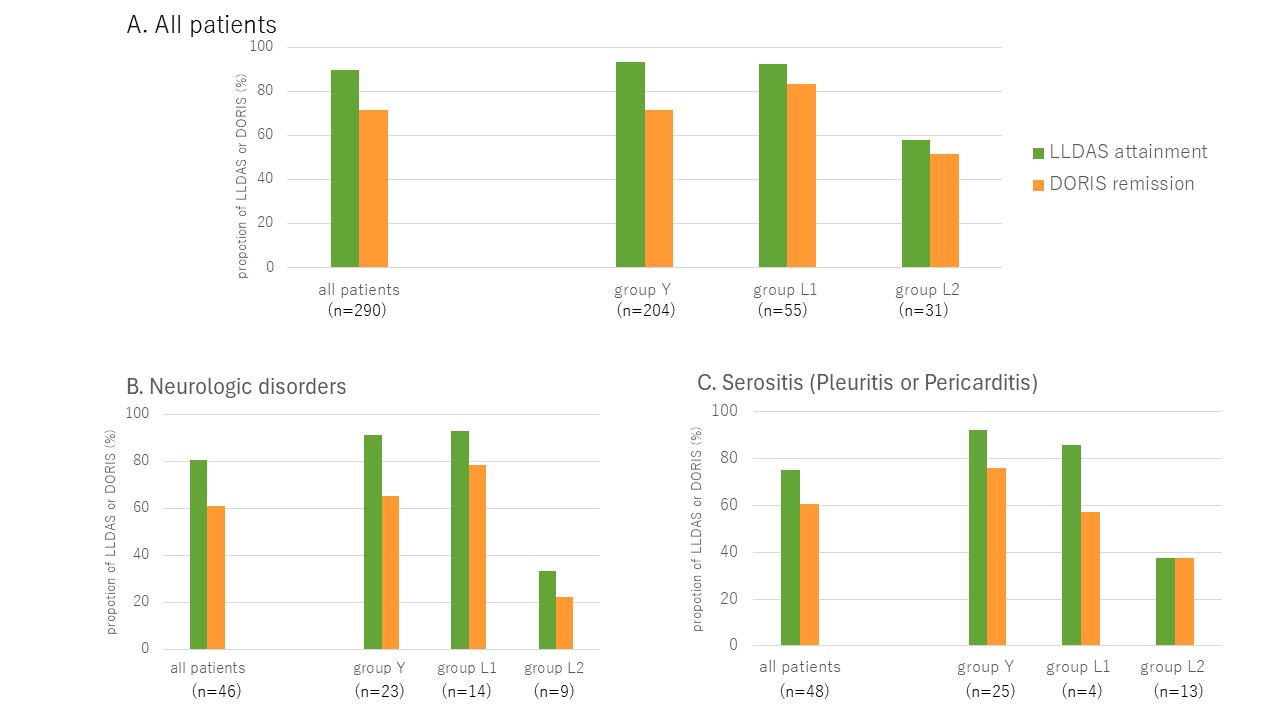
Results: The number of patients in each group (Y, L1, L2) diagnosed with SLE before 2017 was 167, 34, and 5 patients, respectively. Meanwhile, the number of patients in each group diagnosed with SLE since 2018 was 47, 24, and 28 patients, respectively, showing an increase in the number and proportion of late-onset SLE patients in recent years (Figure 1). The table showed the male SLE was significantly more prevalent in the group L1+L2, with the highest proportion observed in the L2 group. Group L1+L2 had significantly more serositis (pleuritis or pericarditis) and neurologic disorders, with 51% of group L2 patients having serositis, while significantly less facial erythema, discoidal rash, and photosensitivity than group Y. Regarding treatment, prednisolone maintenance doses were compared according to age; LLDAS attainment and DORIS remission rates tended to be lowest in the L2 group (Figure 2) . For NPSLE, LLDAS attainment rates in each group (Y, L1, L2) were 78%, 69%, and 33%, respectively, and DORIS remission rates were 65%, 78%, and 22%, respectively, indicating that group L2 had difficulty reducing glucocorticoid. Group L2 had a poor prognosis due to difficulties in continuing immunosuppressive therapy such as cyclophosphamide, complications such as infection and heart, liver, and kidney dysfunction, and higher mortality due to primary disease or infection. Of the 13 patients in the L2 group who did not achieve LLDAS, 8 died during the observation period, and 4 were transitioned to palliative care.
Conclusion: Very late-onset SLE patients diagnosed over the age of 70 may be increasing in recent years, and their clinical manifestations are atypical, such as the absence of skin rash. SLE cases with serositis and CNS symptoms should be differentiated from SLE, and the increasing proportion of male SLE patients should be noted. Further studies are needed on the treatment of older SLE patients, as they are more likely to have multiple comorbidities and are more prone to adverse events.
The relative risk ratios between groups Young-onset (group Y) and Late-onset (group L) were analyzed, with significant results highlighted in bold*.
(A) shows the proportion of LLDAs or DORIS remission of all patients (n=290) and classified by group Y, L1, and L2.
Fifteen out of 305 patients were excluded due to transfer to other hospitals during the study.
(B) and (C) shows the those of the patients with Neurologic disorder (n=46) and Serositis (Pleuritis or Pericarditis )(n=48) , and classified by group Y, L1, and L2.
To cite this abstract in AMA style:
Shirota Y, Oguma M, Kuwata R, Tajima Y, Oka Y, Takeshita M, Kodera T, Ishii T. Clinical Characteristics and Prognosis of Late-onset Systemic Lupus Erythematosus in 305 Japanese Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-characteristics-and-prognosis-of-late-onset-systemic-lupus-erythematosus-in-305-japanese-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-and-prognosis-of-late-onset-systemic-lupus-erythematosus-in-305-japanese-patients/