Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Renal flares are common during treatment of biopsy-proven lupus nephritis (LN). However, it is unknown whether biopsy should be repeated in the event of renal flare. This study aimed to reveal the clinical biomarkers which predict the histologic changes in the repeat renal biopsy during renal flare.
Methods: We evaluated all patients with biopsy-proven LN who underwent repeat renal biopsies at the time of renal flare in Seoul National University Hospital between 2004 and 2018. Renal flare is indicated by an increase in proteinuria, serum creatinine or abnormal urinary sediments. Clinical lupus biomarkers included serum C3/C4, anti-dsDNA antibody level at the time of repeat biopsy. Histologic changes were defined as 1) histologic switch to other ISN/RPS class or alternative pathology, 2) active inflammation (activity index ≥ 7, presence of cellular crescents, interstitial inflammation) and 3) chronic damage (chronicity index ≥ 5, tubular atrophy or interstitial fibrosis). Associations between clinical biomarkers and histologic changes were examined using univariate and multivariate logistic regression analysis adjusting for potential confounding factors.
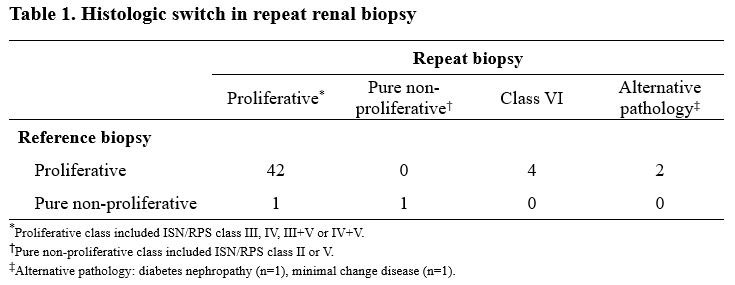
Results: We analyzed 50 pairs of repeat renal biopsy from 46 LN patients with two or more biopsies. The median age was 26 [IQR 18-32] years at reference biopsy and 32 [27-40.7] years at repeat biopsy. 84% was female and the median duration between biopsies was 5.9 years. Of the 50 cases of repeat biopsies, ISN/RPS class switch or alternative pathology was observed in 22 (44%) cases. 6 (12.5%) cases showed histologic switch from proliferative to class VI or alternative pathology, but no pure non-proliferative class. Pure non-proliferative class in the reference biopsy was rare (4%). Low C3 (adjusted odds ratio, 0.04; 95% CI, 0.002 to 0.41; P=0.02) or increased anti-dsDNA antibody (adjusted odds ratio, 0.10; 95% CI, 0.009 to 0.96; P=0.05) was associated with lower conversion rates of proliferative to class VI or alternative pathology at renal flare. In addition, low C3 was associated with higher activity index (adjusted odds ratio, 19.83; 95% CI, 2.05 to 191.57; P=0.01) and presence of cellular crescent (adjusted odds ratio, 10.73; 95% CI, 1.11 to 104.04; P=0.04), while serum creatinine was associated with advanced tubulointerstitial damage at renal flare (adjusted odds ratio, 2.62; 95% CI, 1.25 to 5.46; P=0.04).
Conclusion: Low C3 at renal flare is associated with the retention of proliferative class and active glomerular inflammation at renal flare in patients with originally proliferative LN. These results support C3 as a surrogate marker to distinguish active LN from change to class VI or alternative pathology at renal flare. Hence, it will be helpful for making decisions about repeat renal biopsy or immunosuppressive therapy.
To cite this abstract in AMA style:
Kim M, Lee H, Song Y, Lee E. Clinical Biomarkers at Renal Flare Are Associated with Histologic Changes in Repeat Renal Biopsy in Patients with Biopsy-proven Lupus Nephritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/clinical-biomarkers-at-renal-flare-are-associated-with-histologic-changes-in-repeat-renal-biopsy-in-patients-with-biopsy-proven-lupus-nephritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-biomarkers-at-renal-flare-are-associated-with-histologic-changes-in-repeat-renal-biopsy-in-patients-with-biopsy-proven-lupus-nephritis/