Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Pericarditis is an important feature in the classification criteria and disease activity assessments in Systemic Lupus Erythematosus (SLE). We aimed to study the prevalence, outcomes, and associations of pericarditis.
Methods: This is a retrospective study of patients with pericarditis identified from a single-center SLE clinic database. The diagnosis of pericarditis was based on the definition of SLEDAI-2K. The prevalence of pericarditis was determined in both inception (enrolled within one year of diagnosis) and prevalent cohorts. Demographic and clinical parameters in the inception cohort were retrieved. The outcomes of pericarditis were defined as acute (resolution < 3 months), chronic (lasting ≥ 3 months), and relapse (recurrence after complete resolution). Variables associated with pericarditis were analyzed within the inception cohort. Factors associated with the outcome of pericarditis (acute versus chronic) were examined within the pericarditis subgroup. Descriptive analysis of the data with univariate and multivariate (MV) analyses was conducted. Two models, one with patient characteristics and the other with autoantibodies, were used.
Results: Pericarditis was identified in 428 of 2122 patients (20.16%) [205 of 900 (22.8%) in the inception and 223 of 1222 (18.2%) in the prevalent cohorts].
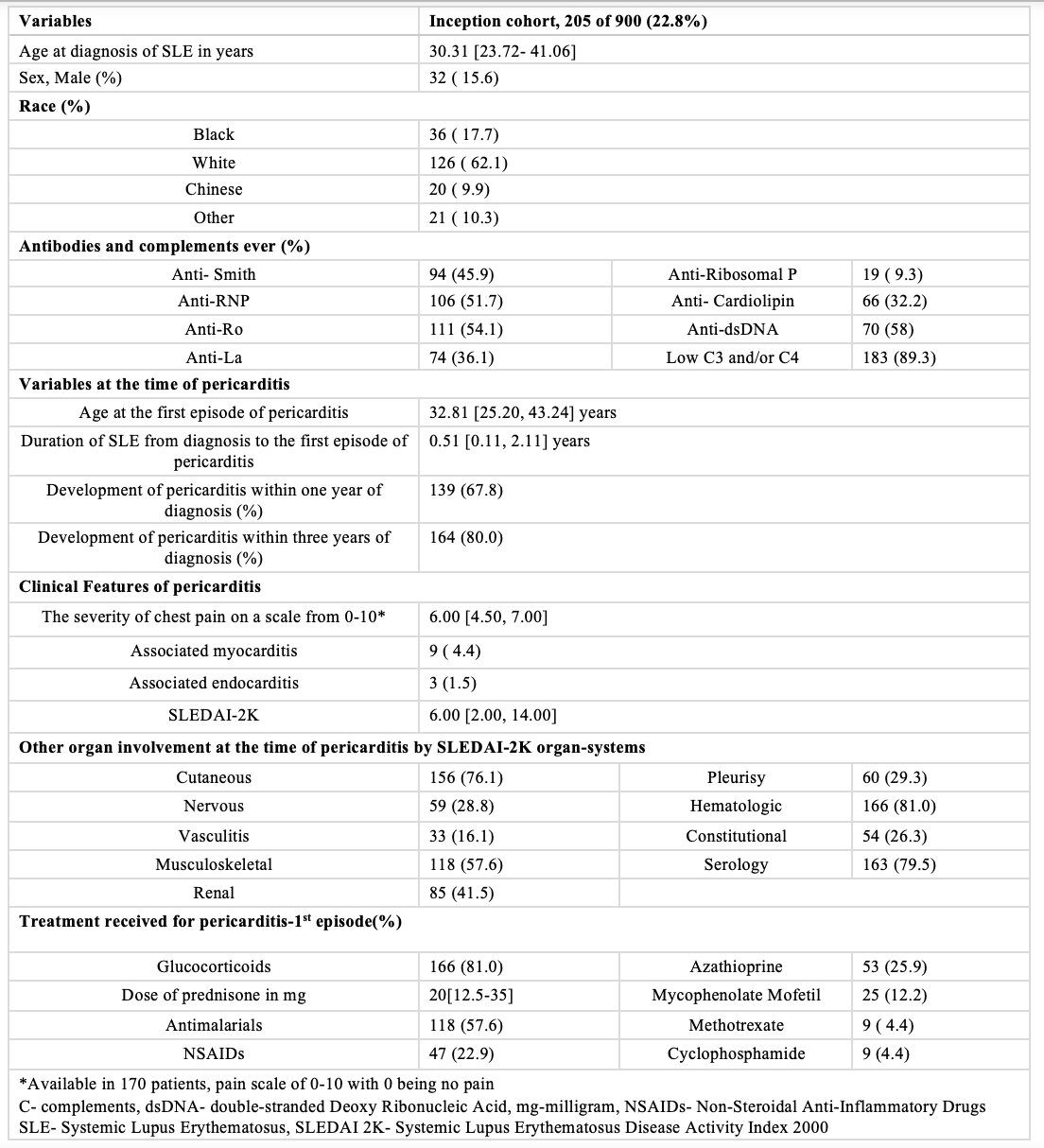
In the inception cohort, age at SLE diagnosis was 30.31 years (IQR 13.72-41.06) with a Female-to-Male ratio of 5.4:1 (Table 1). The age at pericarditis was 32.31 years (IQR 25.2-43.24), and it typically developed early in the disease course, with a median disease duration of 0.51 years (IQR 0.11-2.11) at the first episode. In 170 patients, the severity of chest pain at presentation was 6.5 (IQR 4.25-8). Associated myocarditis was observed in 4.4% and endocarditis in 1.5%.
SLEDAI-2K at the time of pericarditis was 6 (2–14), with commonly affected organ systems being hematologic (81%), skin (76.1%), musculoskeletal (57.6%), and renal (41.5%). The majority of patients had low complements and/or elevated anti-dsDNA (79.5%). Treatment primarily involved oral steroids (81%), and antimalarials (57.6%), with the most common immunosuppressant used being azathioprine (25.9%).
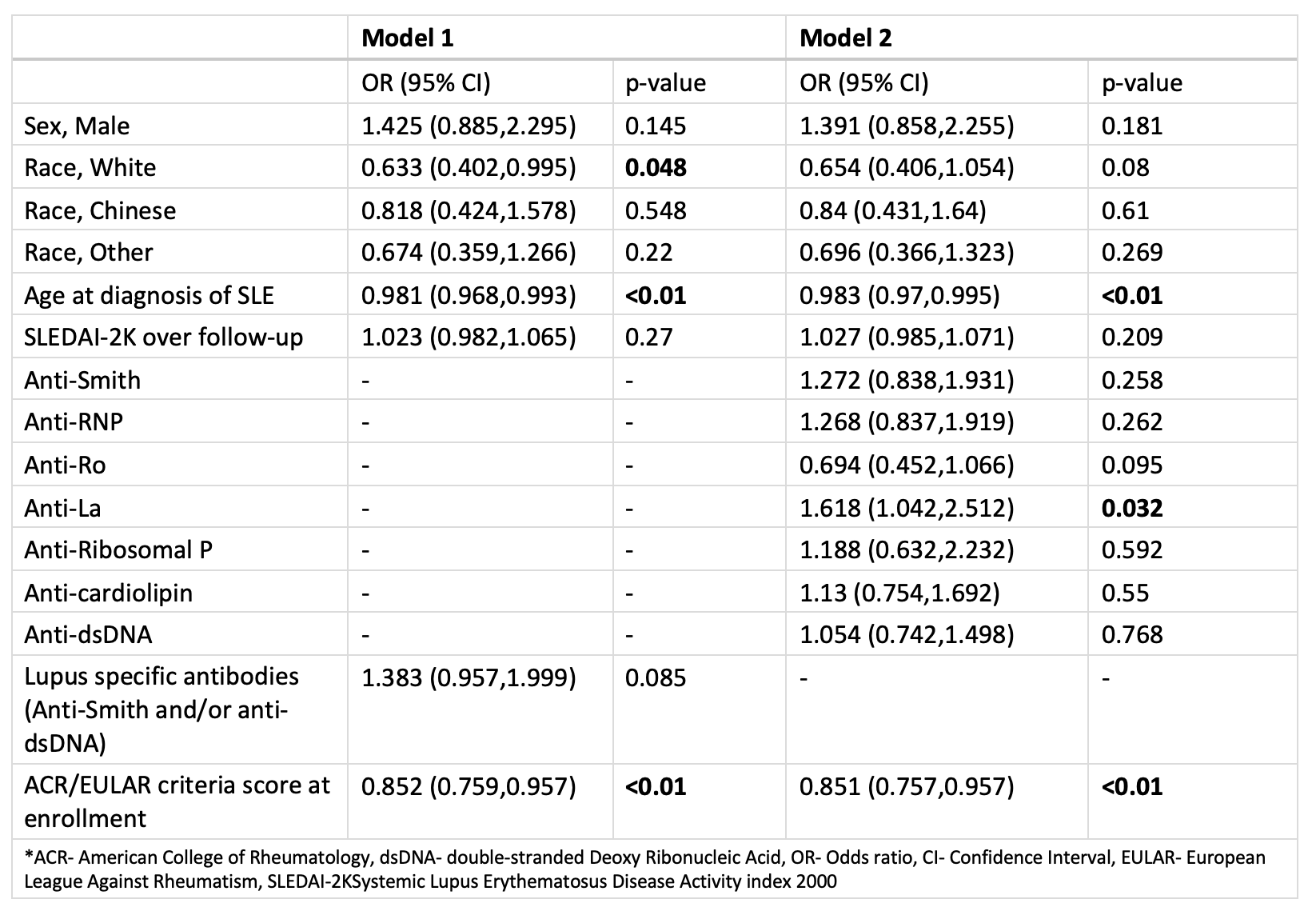
Pericarditis was associated with a younger age, white race, anti-La (SSB) antibodies, and lower baseline ACR scores across two models when compared with patients without pericarditis. (Table 2)
The outcomes were favorable for most, with 79.5% achieving complete resolution within 3 months. Chronic pericarditis was observed in 15.6% for a duration of 4.59 (3.3–16.78 months). Relapses occurred in 19.5% of patients, with a median of two relapses (IQR 2–3) (Figure 1). No associations with sex, race, age at diagnosis, disease duration at the time of the episode, SLEDAI-2K, lupus-specific antibodies, use of NSAIDs, or immunosuppressants were found for those with chronic pericarditis.
Conclusion: Pericarditis was observed in 20.16% of the cohort with the majority resolving within 3 months. It was typically seen early in the disease course and associated with active disease in other organ systems.
To cite this abstract in AMA style:
Mehta P, Kharouf F, Li Q, Whittall Garcia L, Gladman D, Touma Z. Clinical Associations and Outcomes of Pericarditis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-associations-and-outcomes-of-pericarditis-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-associations-and-outcomes-of-pericarditis-in-systemic-lupus-erythematosus/