Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial Lung Disease (ILD) in patients with Primary Sjögren’s Disease (SjD) is very heterogeneous in terms of pathophysiologic mechanisms, clinical course, radiologic and histologic findings and outcome. Lymphocytic Interstitial Pneumonia (LIP), belonging to the spectrum of benign pulmonary lymphoproliferative disorders, probably represents the most characteristic ILD subset in SjD patients. However, LIP is a rare condition, and very few studies investigated the clinical features of SjD patients with LIP. Therefore, the aim of this study was to characterize the clinical phenotype of LIP patients in a large multicenter SjD-related ILD cohort.
Methods: This was an observational retrospective multicenter study involving patients with diagnosis of primary SjD and ILD documented at least once on High-Resolution Computed Tomography (HRCT). SjD patients with overlapping autoimmune systemic diseases were excluded. For all patients clinical and serologic data were collected according to ESSDAI definitions. Moreover, data regarding pulmonary symptoms, Pulmonary Function Tests (PFT), HRCT pattern defined according to ATS/ERS definitions (Travis et al Am J Respir Crit Care Med. 2013; Raghu et al Am J Respir Crit Care Med. 2022) and respiratory outcome were collected.
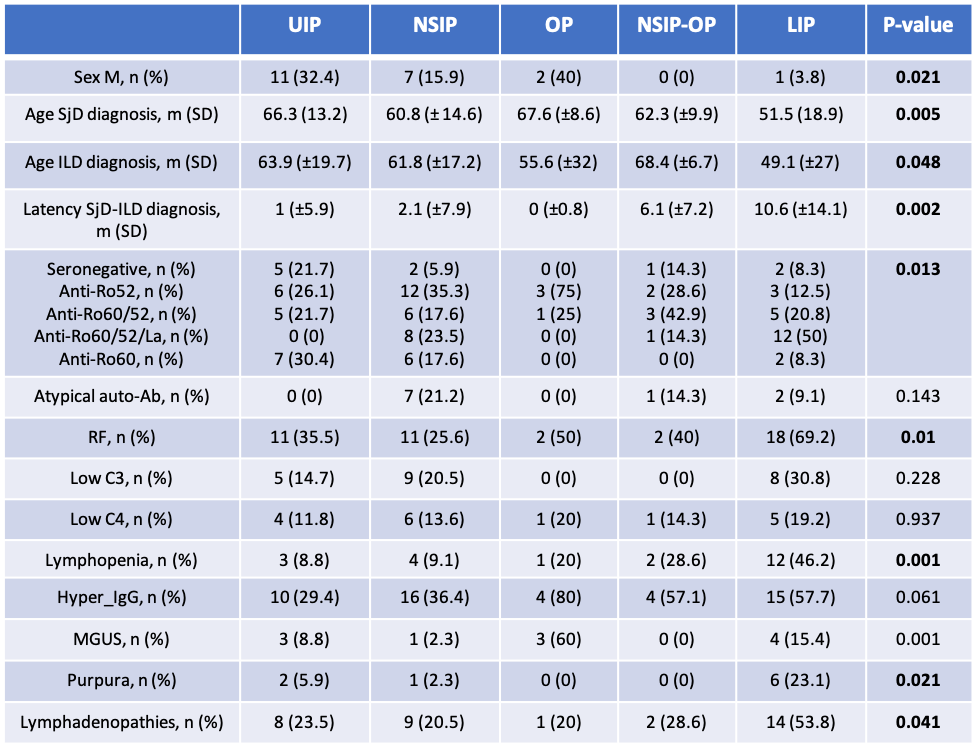
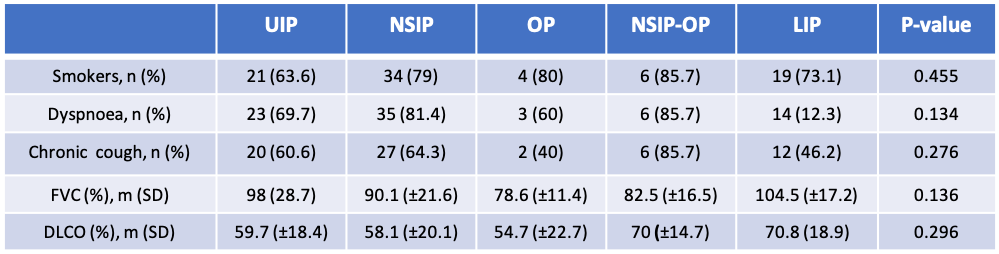
Results: One hundred sixteen SjD-ILD patients were included (M:21=F:95, mean age 60.7±15,7 years). The HRCT pattern was consistent with NSIP in 44 (38%) patients, UIP in 34 (29%), LIP in 26 (22%), NSIP-OP in 7 (6%) and OP in 5 (4%) patients. Mean Follow-up time was 5 (±4.8) years and did not differ significantly among patients with different HRCT patterns. Compared to non-LIP, LIP patients were more frequently female (96% vs 78%; p=.04), were younger at the time of SjD diagnosis (51±19 vs 63±14 years; p=.001) and presented a higher prevalence of purpura (23% vs 3%; p=.004), lymphonodal involvement (54% vs 22%; p< .001), triple Ro60/52/La positivity (50% vs 13%; p=.005), RF positivity (69% vs 31%; p=.001) and lymphopenia (46% vs 11%; p< .001). Moreover, LIP patients tended to present more frequently glandular enlargement (23% vs 9%; p=.08), hypergammaglobulinemia (58% vs 38%; p=.077) and preserved FVC and DLCO values on PFT. Finally, for LIP patients it was less common to receive ILD diagnosis before SjD diagnosis (p=.007) and time between SjD and ILD diagnosis was longer (10.6±14 years; p=.001). More details regarding clinical, serologic and pulmonary features of SjD-ILD patients are provided in tables 1 and 2.
On the multivariate analysis, a younger age at the time of SjD diagnosis and RF positivity were the only factors independently associated to LIP pattern.
Conclusion: LIP seems to represent a peculiar ILD phenotype in SjD patients, associated with young age at diagnosis, high systemic disease activity and serologic biomarkers of B-cells hyperactivation, which may represent a promising therapeutic target. SjD patients with LIP present longer latency between SjD and ILD diagnosis, probably due to mild chronic respiratory symptoms, slight impairment of PFT and brilliant clinical response to empiric steroid therapy. Recognizing clinical and serologic characteristics associated to LIP development is key for early suspicion and diagnosis.
UIP= Usual Interstitial Pneumonia; NSIP= Non-Specific Interstitial Pneumonia; OP= Organizing Pneumonia; NSIP-OP= Non-Specific Interstitial Pneumonia- Organizing Pneumonia; LIP= Lymphocytic Interstitial Pneumonia; FVC= Forced Vital Capacity (% of predicted value); DLCO= Diffusion Lung Carbon Monoxide (% of predicted).
To cite this abstract in AMA style:
La Rocca G, Ferro F, Sebastiani M, Manfredi A, Vacchi C, Bartoloni Bocci E, Nicchi M, Atzeni F, Cracò F, Guiducci S, Cometi L, Quartuccio L, Treppo E, manfrè V, Mosca M, Baldini C. Clinical and Serological Characteristics of Sjögren’s Disease-related Lymphocytic Interstitial Pneumonia: A Large Multicenter Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-and-serological-characteristics-of-sjogrens-disease-related-lymphocytic-interstitial-pneumonia-a-large-multicenter-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-serological-characteristics-of-sjogrens-disease-related-lymphocytic-interstitial-pneumonia-a-large-multicenter-study/